Diabetes management is shifting from clinic-based advice to at-home, food-based interventions. Diabetes meal delivery programs are now a critical tool for health plans, public agencies, and community-based organizations aiming to improve health outcomes, close care gaps, and manage total cost of care. These programs move beyond simple food access by integrating medically tailored nutrition, patient engagement, and data monitoring into a scalable, home-delivered model. They solve the persistent challenge of translating dietary guidelines into daily, compliant meals for members and patients.
This guide provides a strategic breakdown of seven leading program models, from prepared meal subscriptions to comprehensive "Food is Medicine" platforms. We analyze their operational frameworks, clinical evidence, and strategic value for payers, providers, and program administrators. For each example, you will find a deep dive into how they work, complete with screenshots and direct links to their platforms. We will cover everything from member onboarding and sample menu design to logistics, patient testimonials, and performance reporting. For organizations offering diabetes nutrition support, a comprehensive understanding of the best sugar alternatives for diabetics is fundamental to meal planning and recipe formulation that drives adherence.
Our goal is to equip you with the insights needed to design, implement, and scale effective nutrition-as-a-benefit initiatives. You will gain actionable takeaways for program design, vendor selection, and operational oversight, helping you find the best platform to meet your population's unique health needs and your organization's strategic goals.
1. Evidence-Based Food is Medicine Programs | Umoja Health
Umoja Health presents a robust, evidence-based "Food is Medicine" program that stands out as a premier choice for organizations seeking scalable and effective diabetes meal delivery programs. Rather than simply providing food, Umoja offers a comprehensive, 12-week turn-key solution designed for rapid activation and measurable results. This model is exceptionally well-suited for health plans, government agencies, and community-based organizations aiming to deploy impactful nutrition interventions without building the infrastructure from the ground up.
The program's core strength lies in its integrated approach, which pairs medically tailored meals and groceries with culturally relevant education and sophisticated outcome analytics. This holistic design targets not just food access but also the critical behavioral and educational components necessary for sustainable diabetes management. The operational backbone, powered by its minority-owned, NMSDC-certified 3PL (Unidad Logistics), ensures compliant, nationwide fulfillment, making it a reliable partner for large-scale public and private sector initiatives.
Strategic Analysis: The Turn-Key Intervention Model
Umoja Health’s platform is engineered for speed and compliance, a critical differentiator for program administrators under tight deadlines or with specific regulatory requirements. The ability to launch a comprehensive program in as little as 60 days provides a significant strategic advantage, enabling partners to address urgent health needs within their populations quickly.
Key Strategic Insight: By bundling medically tailored food, digital education, and reporting into a single package, Umoja removes the operational friction for partners. This allows organizations to focus on member engagement and outcomes rather than logistics, procurement, and compliance management.
The model's flexibility in delivery (at-home or community hub) and its use of culturally appropriate, shelf-stable kits address common barriers to access and engagement, particularly in diverse or rural communities. For instance, a health plan serving a large Hispanic population could deploy kits with familiar staples, increasing the likelihood of program adherence and positive health outcomes. For more information, you can explore Umoja's deep dive into programmatic strategies for improving community nutrition security.
How the Program Works: From Onboarding to Outcomes
The participant journey is designed for simplicity and support, ensuring high engagement from start to finish.
- Onboarding & Enrollment: Partners work with Umoja to define eligibility criteria. Once a member is enrolled, they begin the 12-week program, receiving clear instructions on what to expect.
- Meal & Grocery Delivery: Participants receive regular shipments of medically tailored food boxes. A sample box might include whole grains like quinoa, lean proteins such as canned chicken or beans, low-sodium vegetable broths, and nutrient-dense snacks, all selected to support stable blood glucose levels.
- Digital Education & Engagement: Alongside food delivery, members access virtual tools, including nutrition education modules, healthy recipes, and tips for managing their condition. This digital component reinforces healthy behaviors and provides ongoing support.
- Data Monitoring & Reporting: Umoja provides partners with regular analytics on key performance indicators, such as program uptake, engagement rates, and self-reported health metrics. This data is crucial for demonstrating ROI and refining the intervention.
The integration of these elements creates a powerful feedback loop. For instance, understanding heart-healthy diet principles is crucial for diabetes management, and Umoja’s educational content can be tailored to reinforce these concepts, especially since cardiovascular issues often coexist with diabetes.
Actionable Takeaways for Program Administrators
For payers and public program administrators evaluating diabetes meal delivery programs, Umoja Health offers a replicable and data-driven model.
- For Managed Medicaid Directors: Leverage the 12-week program as a targeted intervention for high-risk members. Use the provided reporting templates to measure changes in key metrics like HbA1c levels or hospital readmission rates, demonstrating clear value to stakeholders.
- For Community-Based Organizations: Partner with Umoja to rapidly deploy nutrition support. The hub-and-spoke delivery model allows you to use your existing community centers as trusted pickup points, increasing access and engagement.
- For Tribal Programs: Utilize the culturally connected kit options to ensure the food provided is both medically appropriate and resonant with your community members, which can significantly boost program uptake and success.
Website: https://umojahealth.com/food-is-medicine
2. ModifyHealth
ModifyHealth carves out a unique space in the world of diabetes meal delivery programs by combining the convenience of fully prepared, heat-and-eat meals with the option for direct clinical support. This platform is ideal for individuals seeking a structured, evidence-based approach to dietary management without the daily burden of cooking, as well as for payers and providers looking for a scalable food-as-medicine intervention. The core of their service is a rotating menu of single-serving, gluten-free entrées designed by dietitians to manage carbohydrate intake and support stable blood sugar levels.
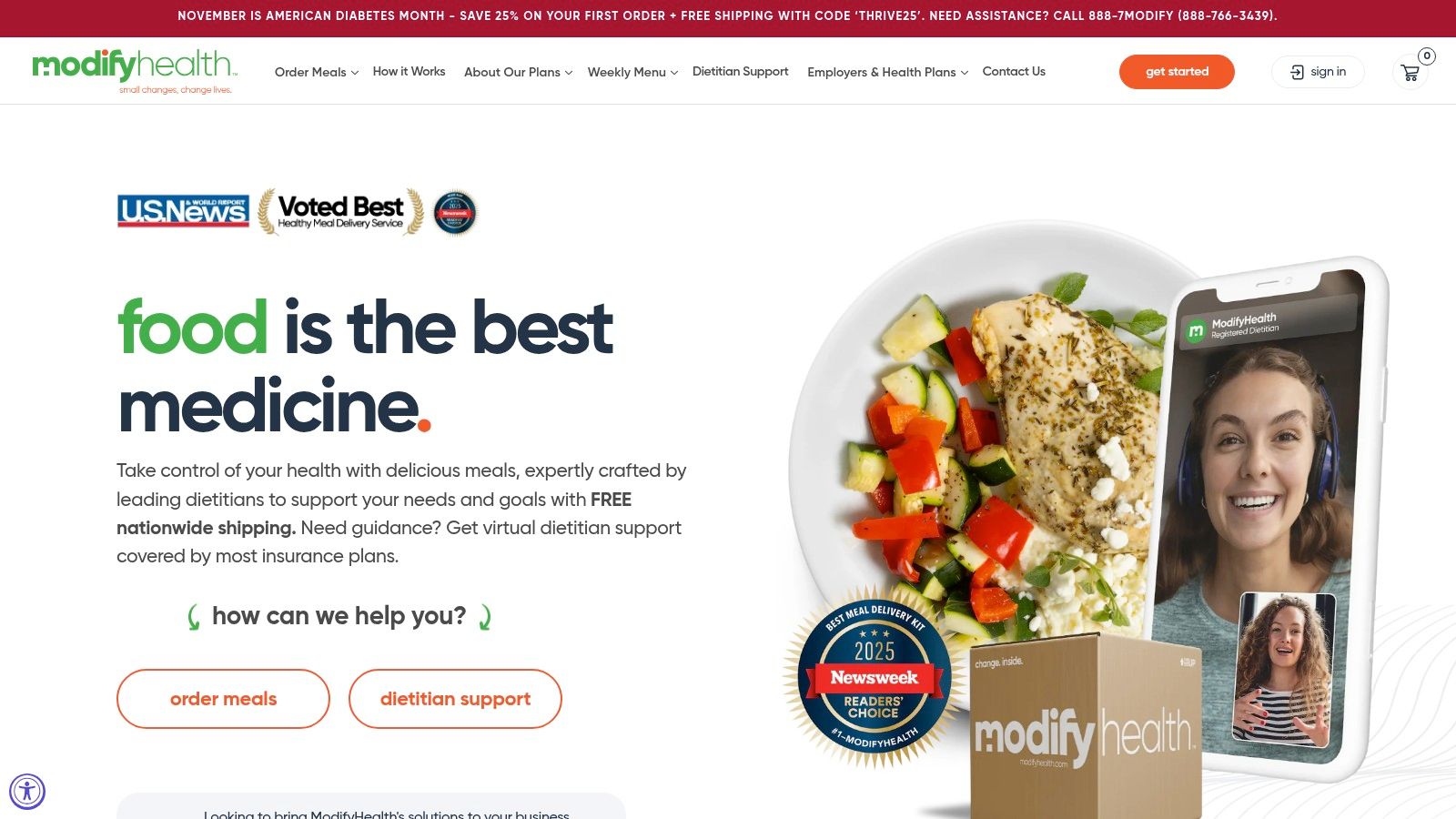
What sets ModifyHealth apart is its optional 6-week FIT (Food-as-Medicine Intervention & Training) program. This integrates the meal delivery service with virtual consultations from registered dietitians, creating a comprehensive support system. This hybrid model provides not just the "what" (the meals) but also the "why" and "how" (the education and personalized guidance), making it a powerful tool for behavior change and improved clinical outcomes.
Strategic Breakdown and Operational Insights
ModifyHealth's model is particularly relevant for Managed Medicaid directors and population health strategists. The platform bridges the gap between a simple meal service and a more intensive medical nutrition therapy (MTN) program, offering a "grocery not MTM" approach that can be easier to implement and scale.
-
Onboarding and User Experience: The process is straightforward. Users select the Diabetes-Friendly plan, choose their meals from a weekly menu, and set up delivery. For those enrolling in the FIT program, the onboarding includes an initial consultation to set goals and personalize the dietary plan. Patient testimonials often highlight the relief of having nutritionally compliant meals readily available, which one user described as "taking the guesswork and stress out of my daily routine."
-
Clinical Integration and Outcomes: The program is designed for data collection and monitoring. Key metrics like A1c levels, weight, and blood pressure can be tracked, providing tangible evidence of the program's impact. This makes it an attractive option for payers seeking to demonstrate ROI through improved health outcomes and reduced healthcare utilization.
-
Menu and Logistics: Sample menu items include Blackened Salmon with Quinoa & Broccoli and Lemon Thyme Chicken with Roasted Potatoes & Green Beans. Each meal is clearly labeled with nutritional information. Operationally, the single-serving, pre-packaged format simplifies kitting and cold-chain logistics for their fulfillment partners, ensuring consistent quality and food safety during home delivery.
Pricing and Access
ModifyHealth operates on a flexible weekly subscription model.
| Feature | Details |
|---|---|
| Pricing | Entrées are priced individually, typically around $12.95 per meal. |
| Minimum Order | There is a 6-meal minimum per weekly order. |
| Shipping | Shipping fees may apply, though promotional offers for free shipping are frequent. |
| Insurance Coverage | A key differentiator is that ModifyHealth meals may be covered by certain insurance plans or Medicare Advantage plans in specific states, positioning it as a medically-integrated service. |
| Website | https://modifyhealth.com |
This model provides a clear pathway for payers to offer a medically-tailored meal benefit that is both clinically robust and operationally efficient.
3. Mom’s Meals
Mom’s Meals is a major player in the medically tailored diabetes meal delivery programs space, focusing on accessibility and affordability. They provide fully prepared, refrigerated meals designed by dietitians to meet specific nutritional guidelines, including those aligned with the American Diabetes Association (ADA). This service is particularly valuable for health plans, Medicare/Medicaid programs, and self-paying individuals seeking a reliable, no-prep solution for managing chronic conditions like diabetes. Their model emphasizes broad reach and operational scale, shipping nationwide to serve diverse populations.
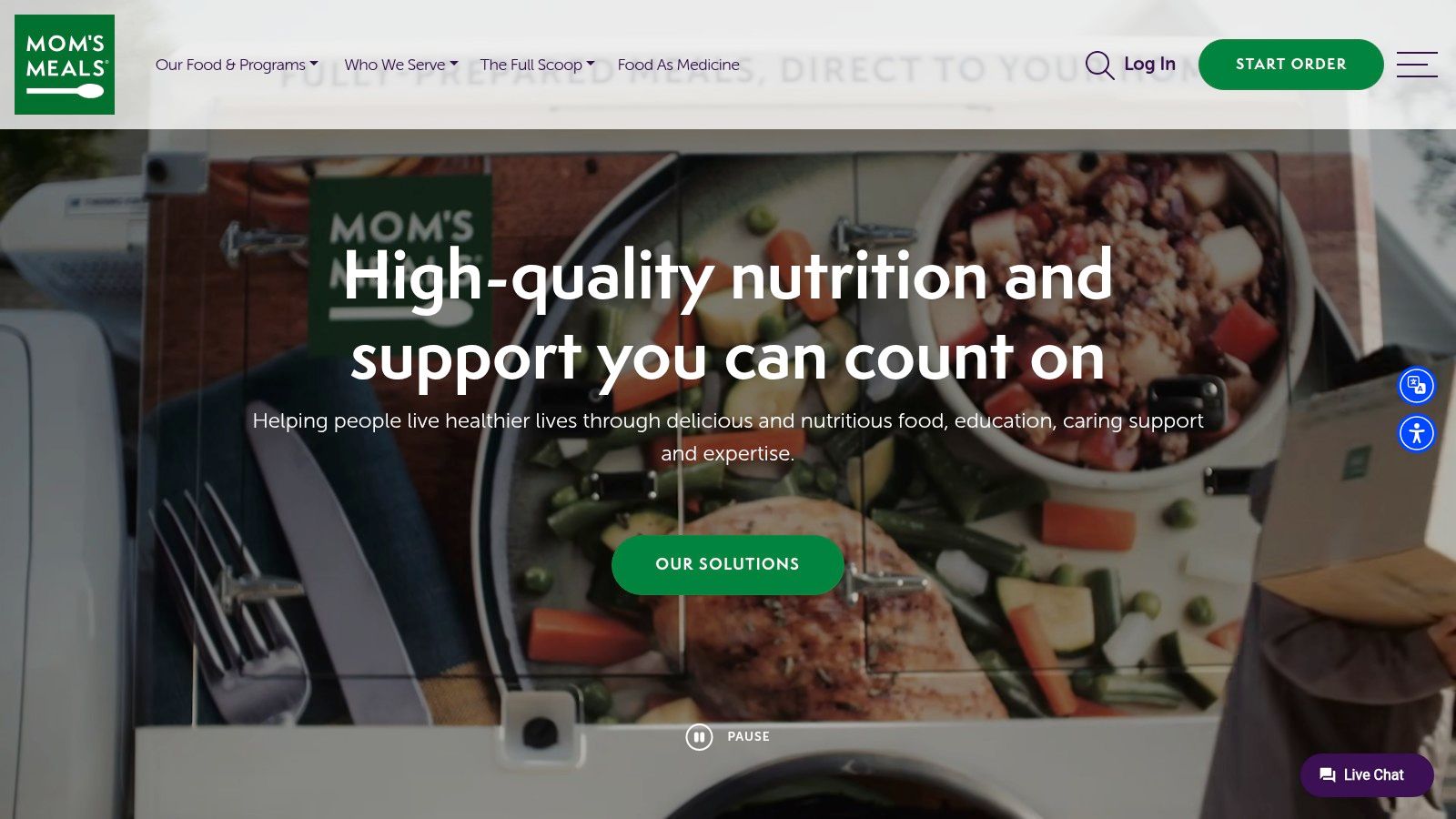
What distinguishes Mom’s Meals is its deep integration with the healthcare system. It is one of the most widely available options offered as a benefit through Medicare Advantage, Medicaid, and other health insurance plans. This positions it as a key partner for payers aiming to provide a food-as-medicine benefit that is both cost-effective and easy for members to use, removing the significant barrier of out-of-pocket costs for eligible individuals.
Strategic Breakdown and Operational Insights
For population health directors and MCOs, Mom’s Meals offers a scalable, turn-key solution for deploying a medically tailored meal benefit. The service is designed for simplicity and compliance, addressing the logistical challenges of providing consistent nutritional support to large member populations.
-
Onboarding and User Experience: Members or customers can sign up directly or are referred through their health plan. The process involves selecting the Diabetes-Friendly menu and choosing from a large, rotating selection of meals. The meals arrive refrigerated and can last up to 14 days, reducing delivery frequency. A user testimonial often cited the convenience, stating, "Having the meals ready in the fridge just takes one big worry off my plate every day."
-
Clinical Integration and Outcomes: The program is built to support health plan goals for managing chronic diseases. By providing nutritionally consistent meals, it helps members maintain stable blood sugar levels, which can lead to improved A1c, reduced hospital readmissions, and better overall health outcomes. The large menu variety across different medical diets (renal, heart-healthy, gluten-free) also allows payers to support members with comorbidities.
-
Menu and Logistics: Sample menu items include Beef Pot Roast with potatoes and carrots, and Cheese Omelet with a side of sausage and potatoes. Each meal is clearly labeled with nutritional facts. Operationally, their nationwide cold-chain logistics are highly developed, ensuring that meals are delivered safely and maintain their quality. The 14-day refrigerated shelf life simplifies inventory management for both the company and the end-user.
Pricing and Access
Mom’s Meals offers a straightforward model for both direct consumers and health plan members.
| Feature | Details |
|---|---|
| Pricing | Self-pay meals are priced individually, starting at $7.99 per meal. |
| Minimum Order | A minimum of 10, 14, or 21 meals per delivery is typical. |
| Shipping | A flat shipping fee applies to self-pay orders, though subscription discounts can sometimes offset this cost. |
| Insurance Coverage | This is their core strength. Mom's Meals is a covered benefit under many Medicare Advantage, Medicaid, and Long-Term Services and Supports (LTSS) programs. |
| Website | https://www.momsmeals.com |
This structure makes Mom's Meals an accessible and operationally efficient option for payers looking to implement a wide-reaching, evidence-based nutritional intervention.
4. Diet-to-Go
Diet-to-Go has established itself as a long-standing player among diabetes meal delivery programs, offering a highly structured and convenient solution for individuals managing their condition. The platform is built around its dedicated Balance-Diabetes (Balance-D) plan, which provides fully prepared, calorie-controlled meals designed by dietitians to manage carbohydrate intake and promote stable blood sugar. This service is ideal for those who prefer a straightforward, subscription-based model that removes the daily tasks of meal planning and cooking.
What sets Diet-to-Go apart is its blend of structure and flexibility. Unlike services that offer a fixed number of meals per week, Diet-to-Go allows customers to choose between 5- or 7-day plans and select either two or three meals per day. This customization allows users to tailor the service to their specific lifestyle, whether they need full-week coverage or just support for busy weekdays. The rotating five-week menu cycle also ensures variety, preventing taste fatigue.
Strategic Breakdown and Operational Insights
From an operational perspective, Diet-to-Go's model offers a clear and replicable framework for payers and population health managers aiming to provide a consistent, nutritionally compliant meal benefit. Its long history in the market translates to a refined logistics and customer service process.
-
Onboarding and User Experience: The sign-up process is direct and user-friendly. A new member selects the Balance-D plan, chooses their weekly schedule (number of days and meals), and enters their delivery information. The platform then allows for meal substitutions and customizations, giving users a degree of control. A common sentiment in testimonials is the appreciation for the program's simplicity, with one user noting, "It completely took the stress out of counting carbs and calories for every meal."
-
Clinical Integration and Outcomes: While not a clinical intervention program like ModifyHealth, the service provides a strong foundation for managing dietary intake. The meals are designed to meet American Diabetes Association guidelines for fat and carbohydrates, making them a reliable tool for A1c and weight management. Payers can use this service as a straightforward, scalable benefit to support members' self-management goals.
-
Menu and Logistics: Sample menu items include Porcini Mushroom Chicken and Blackened Salmon with Tropical Salsa. The meals arrive frozen and are designed for quick reheating, a key consideration for operational efficiency. This frozen format simplifies the complexities of food kitting programs and extends the shelf life of the product, reducing food waste and ensuring cold-chain integrity during nationwide shipping.
Pricing and Access
Diet-to-Go uses a transparent weekly subscription pricing structure that varies based on the plan selected.
| Feature | Details |
|---|---|
| Pricing | Costs range from approximately $138 to $226 per week, depending on the number of days and meals chosen. This averages to about $22 per day. |
| Minimum Order | The minimum order is the 5-day, 2-meal-per-day plan. |
| Shipping | A flat-rate shipping fee of $19.98 is applied to each weekly order nationwide. |
| Access | The service is available for direct-to-consumer purchase online, with local pickup options in some metropolitan areas like D.C. and Baltimore. |
| Website | https://diettogo.com |
This straightforward pricing makes it easy for health plans or program administrators to budget for and implement as a supplemental benefit.
5. MagicKitchen
MagicKitchen provides a practical and flexible option within the landscape of diabetes meal delivery programs, focusing on a la carte access to frozen, medically tailored meals. The service is built for individuals who want direct control over their meal choices without the commitment of a recurring subscription. It's an excellent solution for stocking a freezer with portion-controlled, carbohydrate-conscious options, particularly for seniors or those managing chronic conditions at home. The core of their offering is a wide menu of "Diabetic Friendly" entrées, each designed to meet specific nutritional targets for carbohydrates and sodium.
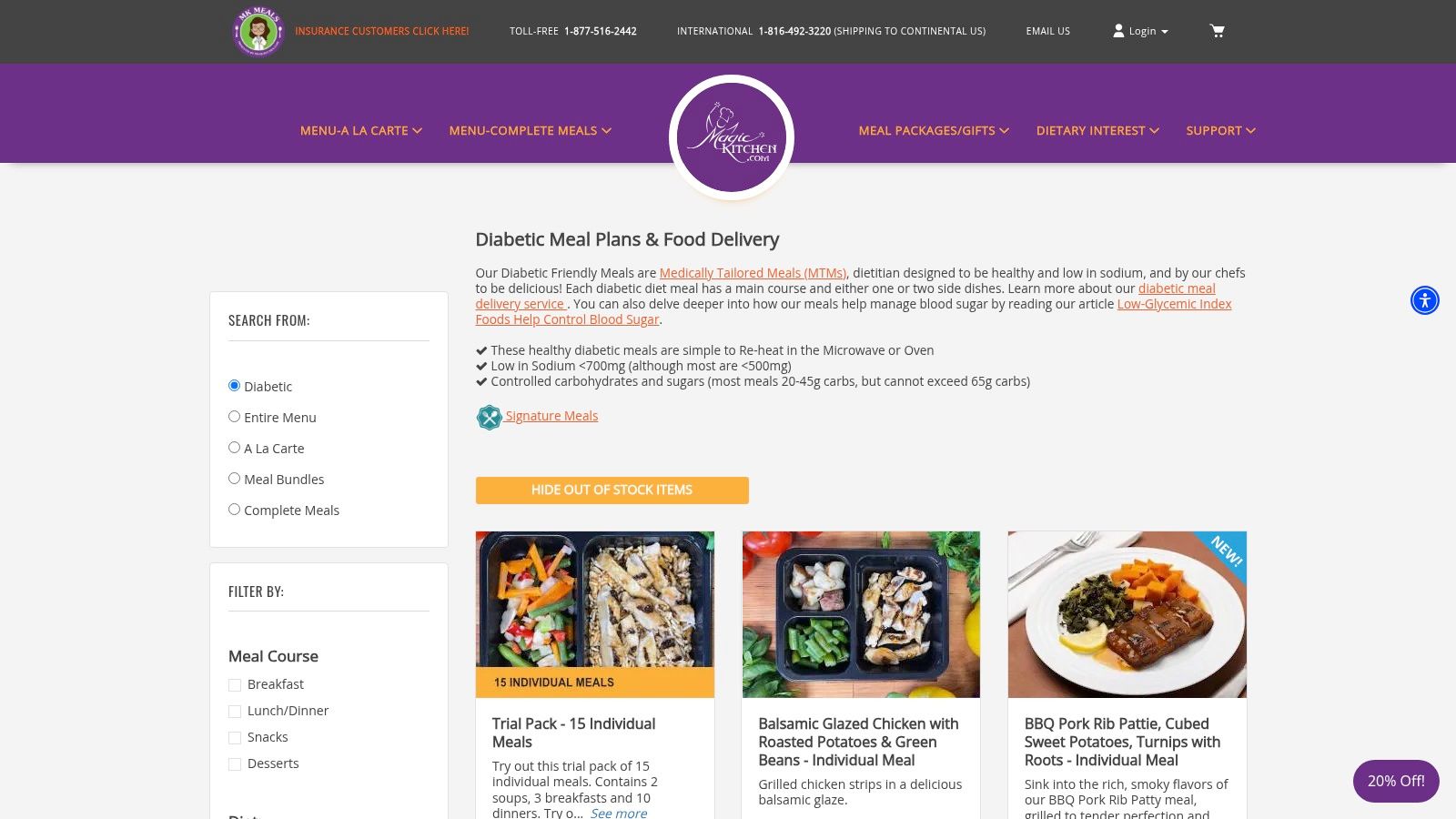
What sets MagicKitchen apart is its consumer-direct, non-subscription model. This approach empowers users to purchase exactly what they need, whether it's a few meals to supplement their weekly cooking or a bulk order to prepare for a busy month. This flexibility makes it a valuable resource for caregivers, individuals recently discharged from a hospital, and health plan members who receive a meal allowance but prefer to choose their own specific entrées rather than receive a pre-set kit.
Strategic Breakdown and Operational Insights
MagicKitchen's model is particularly relevant for payers and program administrators looking for straightforward, scalable solutions for providing medically tailored meals. The a la carte system simplifies benefit administration, allowing members to use a debit card or allowance to procure compliant meals directly.
-
Onboarding and User Experience: The process is as simple as online grocery shopping. Users navigate to the "Diabetic Friendly" menu, add individual items to their cart, and check out. While the website interface is more traditional, its directness is a key feature. A user testimonial noted, "I appreciate that I can just order the half dozen meals my husband actually likes. No subscription, no unwanted items." This highlights the value of choice in driving patient satisfaction and reducing food waste.
-
Clinical Integration and Outcomes: While not a clinical program with built-in monitoring, MagicKitchen provides the essential tools for self-management. Every meal has clear, accessible nutritional information, enabling individuals and their dietitians to easily track intake of carbohydrates, sodium, and calories. This supports adherence to a prescribed dietary plan.
-
Menu and Logistics: Sample menu items include Beef Pot Roast with roasted potatoes and vegetables, and Salmon & Vegetable Linguini. The company’s operational strength lies in its frozen fulfillment logistics. Meals are flash-frozen and shipped with dry ice, ensuring they arrive ready for freezer storage. For health plans considering logistics, MagicKitchen's fulfillment strategy showcases a robust cold-chain solution for direct-to-consumer delivery.
Pricing and Access
MagicKitchen's pricing is transparent, with costs based on the specific items chosen.
| Feature | Details |
|---|---|
| Pricing | Entrées are priced individually, generally ranging from $12 to $15 per meal. Bundles and meal packs offer potential savings. |
| Minimum Order | There is no strict meal minimum, but shipping costs are structured to encourage larger orders. |
| Shipping | Shipping is a separate charge and varies by weight and distance; free shipping is often available over a certain threshold (e.g., $100). |
| Insurance Coverage | MagicKitchen is a registered provider for some Medicare Advantage, long-term care, and waiver programs, allowing members to use their benefits. |
| Website | https://www.magickitchen.com/menu/MK-meals-diabetic.html |
This direct-to-consumer, a la carte model offers a scalable and member-centric approach for payers aiming to provide a flexible food-as-medicine benefit.
6. Sunbasket
Sunbasket addresses the needs of individuals managing diabetes by offering a hybrid model that blends the hands-on experience of meal kits with the convenience of pre-made meals. This platform is an excellent fit for those who enjoy cooking with whole-food ingredients but also require quick, heat-and-eat options for busier days. By providing clear "Diabetes-Friendly" and "Carb-Conscious" filters, Sunbasket empowers users to take an active role in their dietary management, making it one of the more flexible diabetes meal delivery programs available.
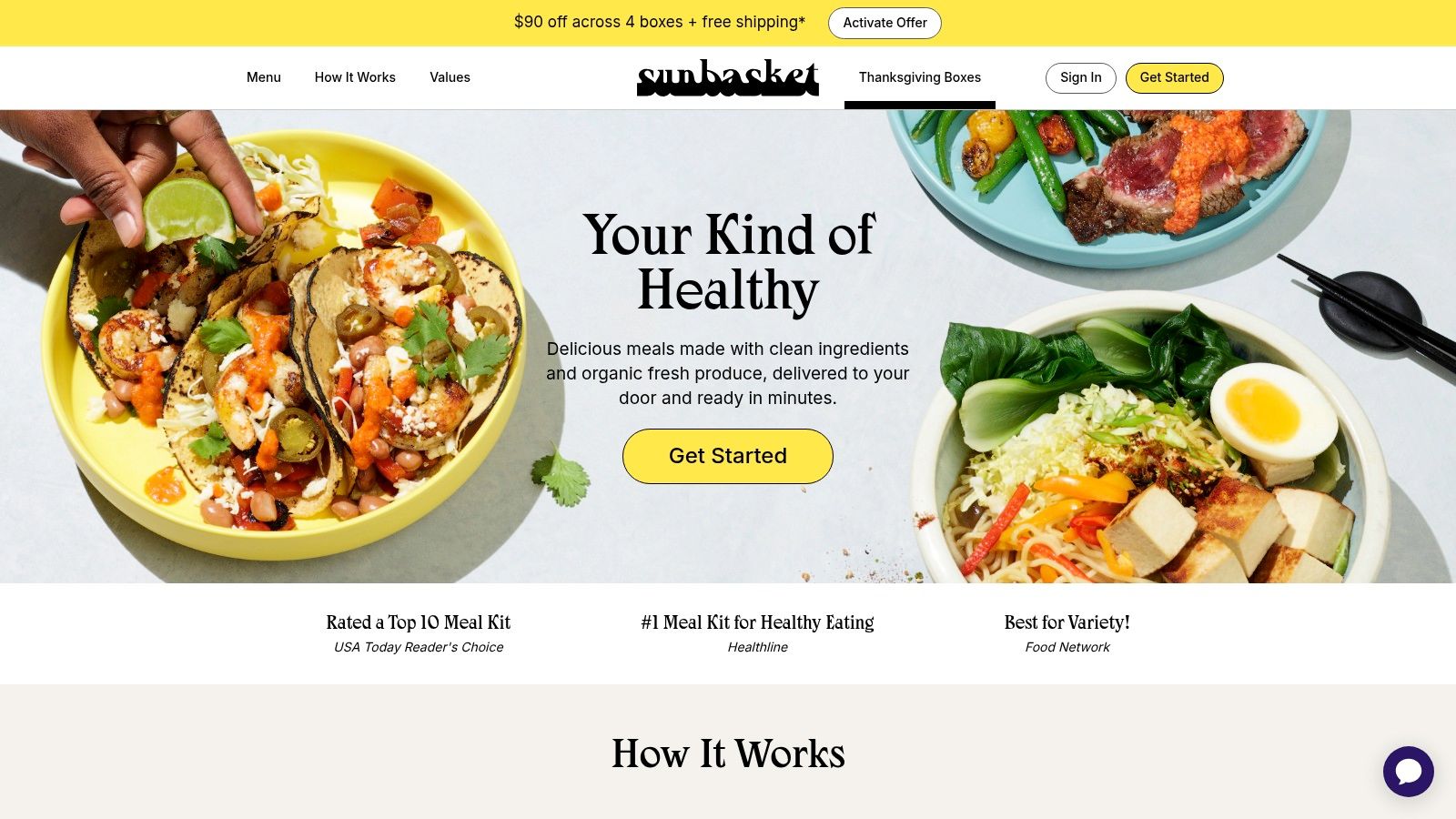
The service stands out by giving users granular control over their weekly menu, allowing them to mix and match meal kits with single-serving "Fresh & Ready" items in a single delivery. This unique approach supports skill-building in the kitchen while providing a reliable backup of nutritionally compliant meals. For individuals aiming to build sustainable healthy eating habits, Sunbasket provides both the ingredients and the blueprint for success.
Strategic Breakdown and Operational Insights
Sunbasket's model offers a compelling option for population health programs focused on engagement and education. The meal kit component actively teaches portion control and healthy cooking techniques, which can lead to long-term behavior change beyond the subscription period. It provides a less clinical, more lifestyle-oriented intervention.
-
Onboarding and User Experience: Users select the Diabetes-Friendly plan or apply the corresponding filter during meal selection. The interface clearly displays nutritional information, including net carbs, for each recipe or prepared meal. One member noted, "I love that I can learn to cook the diabetes-friendly recipes myself, and on nights I'm too tired, the Fresh & Ready meals save me from making bad choices." This feedback highlights the value of its hybrid format.
-
Clinical Integration and Outcomes: While not a formal "food-as-medicine" program with dietitian support like some competitors, Sunbasket's Carb-Conscious plan is designed to align with clinical dietary recommendations, targeting 25-35g of net carbs per serving. This structure provides a tangible framework for members to manage blood sugar through diet, which can be tracked alongside clinical markers like A1c by their healthcare providers.
-
Menu and Logistics: Sample menu items include Pork Chops with Cherry-Balsamic Sauce and Broccolini or a pre-made Burmese Coconut Chicken Noodle Soup. The combination of meal kits (with pre-portioned ingredients) and prepared meals in a single box requires sophisticated pick-and-pack and kitting operations. This model demonstrates an advanced fulfillment strategy that accommodates diverse product formats while ensuring ingredient freshness and cold-chain integrity across a broad delivery network.
Pricing and Access
Sunbasket uses a weekly subscription model where pricing is based on the specific meals selected.
| Feature | Details |
|---|---|
| Pricing | Meal kits start around $11.49 per serving; Fresh & Ready meals start at $9.99. |
| Minimum Order | A weekly minimum order value, typically around $65, is required to ship. |
| Shipping | Shipping fees may apply, but promotional offers for free shipping on the first order are common. |
| Availability | Delivers to most of the contiguous U.S. but excludes Alaska, Hawaii, Montana, and parts of New Mexico. |
| Website | https://sunbasket.com |
This pricing and delivery structure makes Sunbasket a scalable option for programs aiming to provide a high-quality, engaging, and educational food benefit that encourages active participation in health management.
7. bistroMD
bistroMD stands out in the diabetes meal delivery programs landscape with its strong clinical foundation, founded by a physician to specifically address metabolic health through diet. The service provides a dedicated Diabetes-Friendly program featuring a wide variety of doctor-designed, chef-prepared frozen meals. This platform is an excellent choice for individuals who want the structure of a complete meal plan backed by medical expertise, offering a convenient, long-term solution to managing blood sugar through nutrition.
The core principle behind bistroMD is providing nutritionally balanced, portion-controlled meals that are low in carbohydrates and high in lean protein. This approach helps promote stable glucose levels and satiety. Beyond the meals, members gain access to support from registered dietitians, reinforcing the program's commitment to being a comprehensive tool for diabetes management, not just a food delivery service.
Strategic Breakdown and Operational Insights
For population health managers, bistroMD's model offers a clear, scalable intervention that emphasizes clinical validity and ease of use. The frozen meal format simplifies logistics while the extensive, rotating menu helps with long-term member adherence.
-
Onboarding and User Experience: The sign-up process guides users to select the Diabetes-Friendly plan and then choose their program cadence (e.g., 5-day or 7-day plan, with or without breakfasts). Members can then customize their weekly menu from a large catalog of over 100 options. One member noted, "Having the meals planned and delivered took away the daily stress of carb counting and cooking, which was a huge relief."
-
Clinical Integration and Outcomes: The program is built on principles of medical nutrition therapy, with each meal designed to contain fewer than 25 grams of net carbohydrates. This strict nutritional guardrail makes it a reliable tool for payers tracking member outcomes like A1c reduction and weight management. The availability of dietitian support provides a mechanism for personalized guidance and behavior reinforcement.
-
Menu and Logistics: Sample meals include Tilapia with a Red Pepper Coulis and Pork Tenderloin with Mushroom Marsala. The frozen, single-serving format is ideal for large-scale distribution, ensuring product consistency and simplifying cold-chain management for nationwide delivery. This predictability is a key operational advantage for health plans implementing a meal benefit.
Pricing and Access
bistroMD uses a straightforward weekly subscription model with clear, upfront costs.
| Feature | Details |
|---|---|
| Pricing | Starts at approximately $9.50 per meal, with the final cost depending on the specific plan selected. |
| Minimum Order | Plans typically include 10 to 21 meals per week (lunches and dinners for 5 or 7 days, plus optional breakfasts). |
| Shipping | A flat shipping fee of $19.95 is applied to each weekly delivery across the contiguous U.S. |
| Insurance Coverage | While direct insurance billing is not standard, members may be able to use HSA/FSA funds for the program. |
| Website | https://www.bistromd.com |
This pricing structure offers a predictable, all-in-one solution for individuals and payers seeking a clinically robust, ready-to-eat meal program.
Diabetes Meal Delivery Programs — 7-Provider Comparison
| Service | Implementation complexity | Resource requirements | Expected outcomes | Ideal use cases | Key advantages |
|---|---|---|---|---|---|
| Evidence-Based Food is Medicine Programs (Umoja Health) | Moderate — turn‑key partner onboarding and contracting (launch ~60 days) | Partner contracts/funding, logistics & reporting integration, distribution network | Measurable 12‑week diabetes risk reduction and improved management | Health plans, CBOs, food banks, government/tribal programs seeking rapid, scalable interventions | Rapid activation, medically tailored meals + education + analytics, culturally adapted, FDA‑registered 3PL |
| ModifyHealth | Low — consumer-facing with optional program integration | Per‑meal budget, weekly ordering, optional virtual RD time; variable insurance pathways | Improved meal adherence and short‑term glucose control with dietitian support | Individuals wanting dietitian‑designed heat‑and‑eat meals and guided short programs | Dietitian‑designed entrées, flexible weekly orders, optional RD consults, possible insurance coverage |
| Mom’s Meals | Low — widely available with insurer integrations | Self‑pay or benefit coverage, refrigerated storage, subscription optional | Affordable medically tailored meals leading to better adherence and clinical support | Members of Medicare Advantage/Medicaid/health plans or cost‑sensitive consumers | Affordable pricing, broad insurer integration, large medically tailored menu |
| Diet‑to‑Go | Low — straightforward subscription model | Subscription cost, frozen storage, weekly shipping fee | Structured, consistent diabetes‑specific meal plan adherence | Consumers wanting a subscription with multiple cadence and menu options | Dedicated Balance‑Diabetes plan, multiple scheduling choices, competitive per‑meal pricing |
| MagicKitchen | Low — a la carte ordering, no subscription required | Freezer space, potential higher dry‑ice shipping on small orders | Convenient freezer stock of carb/sodium‑controlled entrées for intermittent use | Buyers who want to pick exact meals without subscribing | A la carte control, competitive entrée pricing, bundles and senior/medical program support |
| Sunbasket | Moderate — meal‑kit prep plus ready‑meal mix; subscription min. | Subscription minimum, home cooking time/tools, fresh ingredient delivery | Improved whole‑food intake and cooking skills with explicit carb targets | People preferring whole‑food cooking or mixed kits + ready meals | Whole‑food focus, clear carb‑conscious labeling, ability to mix kits and ready meals |
| bistroMD | Low — subscription frozen meals with clinical framing | Subscription cost, frozen storage, optional RD support | Predictable, clinically framed nutrition to support diabetes management | Consumers seeking doctor‑designed, RD‑supported frozen meal programs | Physician‑designed menus, registered dietitian support, extensive diabetes‑focused catalog |
Key Takeaways: Designing and Implementing Your Diabetes Meal Program
Navigating the landscape of diabetes meal delivery programs requires more than just comparing menus and prices. For payers, public program administrators, and health systems, the ultimate goal is to implement a sustainable, effective intervention that drives measurable health outcomes. The programs detailed in this article, from fully prepared meals by Mom's Meals and bistroMD to the flexible grocery-style approach of Sunbasket, illustrate a spectrum of models. The critical first step is to align the program's design with your organization's specific goals and your population's unique needs.
The decision between a prepared meal model and a grocery-style kit is a foundational one. Prepared meals, like those from Diet-to-Go, offer maximum convenience and adherence, making them ideal for members with limited mobility, cooking skills, or time. Conversely, programs offering grocery kits or benefit cards empower members with choice and can build long-term healthy cooking skills, a key factor in sustained behavior change.
Strategic Considerations for Program Implementation
As you move from evaluation to implementation, several strategic pillars are crucial for success. These considerations ensure your program is not just a logistical operation but a powerful clinical tool.
- Compliance and Sourcing: For public programs, adherence to regulations like Buy American provisions is non-negotiable. Work with vendors who can provide clear sourcing documentation. Similarly, understanding specific dietary requirements for programs like Older Americans Act (OAA) or CACFP is essential for vendor selection.
- Logistics and the Cold Chain: The integrity of home-delivered food is paramount. A robust cold-chain management plan, including validated packaging, real-time temperature monitoring, and clear protocols for delivery exceptions (e.g., a member not being home), is a critical operational requirement. This is where a partner with a proven 3PL and sophisticated warehouse management system (WMS) becomes invaluable.
- Member Onboarding and Engagement: A successful program begins with a seamless member experience. As one participant in a Medicaid pilot shared, "Getting the first box was easy, and the welcome call made me feel like someone really cared about my health." This high-touch approach, combining simple enrollment with ongoing nutritional support and check-ins, dramatically improves uptake and long-term engagement.
Measuring What Matters: From Logistics to Outcomes
The true power of modern diabetes meal delivery programs lies in their ability to generate and leverage data. While tracking delivery success and member satisfaction is important, the focus must be on quantifiable health outcomes.
Strategic Insight: Your measurement framework should connect food provision directly to clinical improvement. Go beyond operational metrics and build a robust system for tracking key health indicators to demonstrate ROI and clinical efficacy.
Define your key performance indicators (KPIs) from the outset. Essential metrics to track include:
- Clinical Outcomes:
- Change in HbA1c levels
- Reduction in hospital readmissions and emergency department visits
- Improvements in blood pressure and cholesterol levels
- Utilization and Engagement:
- Program enrollment and retention rates
- Meal redemption and consumption data
- Engagement with supplemental educational resources
- Member-Reported Outcomes:
- Surveys on food security status
- Quality of life assessments
- Program satisfaction and perceived health benefits
By integrating data from claims, electronic health records, and member surveys, you can build a comprehensive picture of your program's impact. This data-driven approach not only justifies the investment but also provides insights for continuous program refinement, ensuring you are delivering the most effective intervention possible. Ultimately, a well-designed program transforms food from a simple provision into a precise, powerful, and evidence-based medical therapy.
Ready to move beyond basic meal delivery and implement a truly integrated Food is Medicine platform? Umoja Health provides the technology and logistics infrastructure to design, manage, and scale evidence-based nutrition programs for complex populations. Explore Umoja Health to see how our platform can help you deliver measurable health outcomes for your members.

