Evidence-based nutrition interventions are strategies and programs that have been proven to work through serious scientific research. This approach moves us beyond stories of success to results we can actually measure and repeat. It's the gold standard for tackling big public health challenges like malnutrition and chronic disease, because it relies on solid data, not just assumptions.
Understanding Evidence-Based Nutrition Interventions
At its heart, taking an evidence-based approach means you are consciously and clearly using the best current evidence to make decisions for people and communities. When a program is being designed—whether it's medically tailored meals for someone with diabetes or nutrition kits for seniors—its goals and structure are shaped by what high-quality studies have already proven.
This method ensures that time, money, and effort go toward strategies with the best chance of actually working. To really get a handle on this, it helps to understand the foundational research methodology that supports these scientific findings. The strength of the evidence is everything, and not all studies are created equal.
The Hierarchy of Evidence
The credibility of any intervention comes down to where its supporting research sits on the "hierarchy of evidence." This is just a simple framework that helps planners and clinicians tell the difference between a promising idea and a rock-solid conclusion.
- Systematic Reviews & Meta-Analyses: This is the top of the pyramid. These studies gather and crunch the numbers from multiple, high-quality randomized controlled trials (RCTs). They give the most complete picture possible.
- Randomized Controlled Trials (RCTs): An RCT is a carefully designed experiment where people are randomly put into either an intervention group or a control group. This is the best way to determine if a specific intervention directly causes a specific outcome.
- Cohort and Case-Control Studies: These are observational studies. They either track groups over time (cohort) or look back to compare groups (case-control) to find links between certain behaviors and health results.
- Expert Opinion and Anecdotal Evidence: While this can be a great source for new ideas, it's the least reliable level of evidence for building large-scale programs because it hasn't been scientifically tested and proven.
The Global Impact of Proven Interventions
You can see why using proven strategies is so important when you look at global public health. Evidence-based nutrition interventions have been at the center of goals set by groups like the World Health Organization. For example, a major target was to cut childhood stunting by 40% by 2025.
Unfortunately, progress has been slow. Projections now show there will still be around 131 million stunted children worldwide, which means we'll miss the target by 27 million. The same is true for anaemia in women, which is on track to be more than double the target level. This just underscores how urgent the need is for effective, scalable programs that we know will work.
At Umoja Health, our own program evaluations show this time and again. Grounding our work in solid evidence is essential for making real progress in https://umojahealth.com/nutrition-security/. This data-first mindset is what lets us design and fine-tune programs that deliver a real, measurable impact.
Core Categories of Nutrition Interventions

To build a program that actually works, you have to understand the main types of evidence-based nutrition interventions. While they all aim to improve health through food, the models, target populations, and the way they deliver services can look very different. Think of these categories as the foundational building blocks for program planners and healthcare providers alike.
From directly providing meals to offering educational support, each strategy has a different level of evidence for specific health outcomes. Knowing these differences is the first step in matching a community's real-world needs with the most effective strategy. This overview will give you a quick framework for the main models you'll come across in the field.
Food as Medicine Models
This is exactly what it sounds like: using food as a direct clinical tool to manage or prevent chronic disease. Two of the most prominent models you’ll see are Medically Tailored Meals (MTM) and Produce Prescription Programs (PPR).
- Medically Tailored Meals (MTM) are fully prepared, nutritionally specific meals for people with complex health issues like congestive heart failure, diabetes, or end-stage renal disease. The research here is strong—rigorous studies have tied MTM to fewer hospital readmissions and lower healthcare costs.
- Produce Prescription Programs (PPR) give patients financial incentives or vouchers to buy fruits and vegetables. The goal is straightforward: increase access to healthy foods and get people eating more of them, especially those who have or are at risk for diet-related diseases.
Population-Focused Interventions
Other evidence-based nutrition interventions are built for specific groups with unique nutritional risks, like children and older adults. These aren't just about handing out food; they often weave in social support and education to tackle multiple health determinants at once.
At Umoja, our own program evaluations have shown us just how critical culturally connected foods are for these models. For example, we design our senior kits not only to be Older Americans Act (OAA) compliant but also to reflect the dietary preferences of the communities we serve. It’s a simple change that makes a huge difference in program uptake and satisfaction.
To help you quickly sort through these common models, the table below breaks down the major intervention categories, their goals, and who they typically serve.
Quick Reference Guide to Nutrition Intervention Types
| Intervention Type | Primary Goal | Target Audience | Common Setting |
|---|---|---|---|
| School/Childcare Programs | Improve diet quality; reduce obesity | Children & adolescents | Schools, childcare centers |
| Senior Nutrition Support | Prevent malnutrition & isolation | Older adults (often 60+) | Congregate sites, homes |
These core categories—from the clinical precision of "Food as Medicine" to broad, population-based support—give you a clear map to start from. When you understand their distinct goals and target audiences, you can align your resources much more effectively and set yourself up for measurable success.
Analyzing Food as Medicine Interventions

When we dig into evidence-based nutrition programs, two "Food as Medicine" models really surface as the most clinically focused and well-researched: Medically Tailored Meals (MTM) and Produce Prescription Programs (PPR). Both are designed to improve health through food, but they get there in very different ways, and the strength of the evidence for each varies. Getting a handle on these differences is critical for any clinician or program planner trying to choose the right strategy.
MTM programs are pretty intensive, providing fully prepared, disease-specific meals to people dealing with complex chronic conditions. PPRs, in contrast, offer financial incentives—usually vouchers or cards—so participants can buy their own fruits and vegetables.
Comparing Clinical Evidence and Outcomes
The research on Medically Tailored Meals is robust and consistently points to strong clinical and financial results. Multiple rigorous studies, including several RCTs, have demonstrated that MTM participants have far lower hospital admission rates—in some cases, a full 50% lower—than control groups. These programs are also tied to a 16% net reduction in healthcare costs, a figure driven mostly by keeping people out of the hospital and the emergency room.
Produce Prescription Programs are also showing great promise, though the body of evidence is still growing and consists more of observational studies than RCTs. The research we have connects PPRs with better food security, higher fruit and vegetable intake, and improved management of key health markers like HbA1c for people with diabetes. While the evidence for direct healthcare cost savings is not yet as strong as it is for MTM, the positive effect on diet quality and patient empowerment is clear. To see how these models fit into the bigger picture, you can explore more on the Food is Medicine movement.
Distilling Lessons for Clinical Practice
The evidence from these studies provides clear recommendations for clinical application. MTM is a high-intensity, high-impact tool best suited for patients with severe, complex diagnoses where strict dietary adherence is critical, such as congestive heart failure, end-stage renal disease, or uncontrolled diabetes. The intervention works by removing barriers of meal preparation and nutritional planning, ensuring clinical precision.
PPRs, on the other hand, are a powerful preventive tool and a lower-intensity intervention. They are an excellent fit for patients at risk for, or in the early stages of managing, chronic diseases who retain the ability and desire to shop and cook. This model focuses on building sustainable healthy habits by empowering patient choice.
Umoja Program Insight: Our own program data validates this tiered approach. We see the best engagement and health outcomes when we direct MTM-style grocery programs to members with multiple comorbidities and recent hospitalizations. In parallel, our PPR models achieve high success in broader community wellness initiatives by making healthy food more accessible and affordable, improving key biometrics over time.
How to Integrate These Interventions
For program planners, turning this evidence into a real-world program takes a structured approach. The key to making these interventions work is matching the right model to the right population—and the right infrastructure.
Here are actionable steps for integration:
- Segment Your Population: Use health data to stratify individuals. Identify the high-acuity, high-cost patient segment for MTM and the moderate-risk segment for PPRs.
- Develop Clear Referral Criteria: Create simple, evidence-based protocols for clinicians. For example: "Post-discharge CHF patients with 2+ comorbidities are eligible for a 12-week MTM program."
- Build a Diverse Partner Ecosystem: For a PPR, this means forging relationships with local grocery stores and farmers' markets. For MTM, it requires partnering with specialized food service providers who can meet complex dietary needs.
- Establish Tiered Success Metrics: Measure what matters for each model. For MTM, track 30-day hospital readmissions and total healthcare costs. For PPRs, monitor voucher redemption rates, food security scores, and biometric data like A1c levels or blood pressure.
Interventions for Vulnerable Populations
Effective nutrition interventions aren't one-size-for-all. You have to tailor them to the specific needs of different age groups. Children and older adults, in particular, face very different nutritional risks that call for specialized, well-researched strategies. For these groups, the best programs always go beyond just handing out food; they weave in social support and education to create real, lasting health improvements.
When you're designing programs for kids, multi-component interventions in schools and childcare centers have the strongest evidence base. These initiatives don't just put healthier food on the plate—they combine it with nutrition education and chances to get active. Numerous studies and systematic reviews show these kinds of programs can significantly reduce childhood obesity rates and improve academic performance. It makes sense: well-nourished kids are ready to learn.
For older adults, the focus shifts to fighting malnutrition and the social isolation that so often comes with it. Programs authorized under the Older Americans Act (OAA), like congregate meals and home-delivered meal kits, are proven winners. The evidence demonstrates they are not just about providing essential nutrition; they’re about creating vital social connections, too.
Best Practices for Serving Children
The evidence is clear: a holistic approach is the only thing that really works. Simply changing a school menu isn't enough. The most successful programs create a supportive environment where healthy choices are the easy choices, reinforced from every direction. You can find more details on how to structure effective child nutrition programs on our website.
Umoja Program Insight: Our own program evaluations back this up completely. When we supply CACFP multi-day kits, we see the highest engagement from childcare sites that also use our nutrition education flyers. That synergy between healthy food and easy-to-understand information is what builds healthy habits early on.
Proven Strategies for Older Adults
For seniors, reliability and accessibility are everything. Home-delivered meal kits are an absolute lifeline for those with limited mobility. Research shows these programs are incredibly effective at reducing hospitalizations and improving overall quality of life by heading off the health problems that come with poor nutrition.
In the same way, congregate meal sites offer more than a hot lunch; they are hubs for community and support. Studies have linked participation in these programs to better nutrient intake and lower rates of depression among seniors. That social interaction is often just as important as the meal itself.
How to Integrate These Interventions
For program planners, turning this evidence into action means getting practical about the target population’s environment and specific needs.
-
For School Programs:
- Partner with educators to integrate nutrition concepts directly into the curriculum, not just the lunch line.
- Engage parents with newsletters, take-home activities, and family taste-test nights to reinforce lessons at home.
- Focus on Environmental Changes: Make water easily accessible and position fruits and vegetables attractively in the cafeteria.
-
For Senior Programs:
- Prioritize Cultural Connection: Offering familiar, well-liked foods dramatically increases consumption and cuts down on waste. Umoja's OAA-compliant kits are designed exactly with this in mind, boosting program adherence.
- Build Robust Delivery Logistics: For homebound seniors, ensure timely, safe, and reliable delivery with temperature controls.
- Integrate "More Than a Meal" Checks: Train delivery drivers to perform simple wellness checks, a proven practice for monitoring for signs of social isolation or declining health.
Implementing Your Nutrition Program
Turning an evidence-based nutrition intervention from a plan on paper into a real-world program is all about operations. Success really hinges on the logistics—getting the right food to the right people, safely and on time. It means sweating the details, from how a meal pack is put together to how it actually lands on a participant's doorstep.
This section is a practical guide for program implementation, zeroing in on the critical details that often get missed. We’ll walk through the best ways to handle meal pack assembly, manage cold-chain needs, get a handle on procurement rules, and set up a last-mile home delivery system that works. Getting each of these pieces right is essential for your program's integrity and for hitting the health outcomes you’re aiming for.
Mastering Kitting and Assembly
The first big operational hurdle is kitting—the hands-on process of assembling individual meal or grocery packs. You can't afford to be sloppy here, especially when you're dealing with hundreds or thousands of boxes. A messy process just creates errors, waste, and higher costs.
A clear, standardized operating procedure (SOP) is non-negotiable. This should include a detailed pack list for every type of kit you offer (like a senior OAA box, a family nutrition pack, or a diabetes-friendly grocery set) and a smart assembly line workflow. At Umoja, we’ve seen firsthand that pre-sorting all the components and using simple visual guides for staff or volunteers dramatically cuts down on packing mistakes and makes the whole process faster.
A few key things for program planners to nail down:
- Create Detailed Pack Lists: Be specific. List every single item, down to the brand and size, so every box is consistent.
- Design an Ergonomic Assembly Line: Lay out your packing stations in a logical flow. You want to minimize how much people have to move around and maximize how many boxes they can pack.
- Implement Quality Control Checks: Set up a final checkpoint to verify the contents before the boxes are sealed. This step is absolutely critical for program fidelity.
Navigating Cold-Chain and Procurement
When your program includes perishable items like fresh produce, milk, or frozen meat, cold-chain logistics become a major factor. Keeping everything at the right temperature from the warehouse to someone's home is a food safety must. This usually means refrigerated trucks, insulated packaging, and tight delivery schedules.
But, there are exceptions that can make your life easier. For example, Ultra-High Temperature (UHT) milk is a shelf-stable option that doesn't need to be refrigerated, which is perfect for multi-day kits in programs like CACFP. Our experience at Umoja confirms that using shelf-stable alternatives where it makes sense can seriously expand a program’s reach into rural or hard-to-serve areas without cutting corners on nutrition.
Procurement adds another layer of complexity, especially if you're working with federal funds.
Navigating requirements like the Buy American provision is a common challenge for SFSP and CACFP sponsors. This rule requires programs to purchase domestically grown and processed foods to the maximum extent practicable. Meticulous vendor selection and documentation are key to compliance.
Designing Last-Mile Home Delivery
The final step, last-mile delivery, is often the trickiest part of the entire operation. This is the journey from your hub to a participant's front door, and it has to be both reliable and affordable. An inefficient delivery system can undo all the hard work that came before it.
Start by mapping out where your participants live to spot dense clusters and remote outliers. This data will be your guide for planning routes and deciding whether to use your own drivers, team up with a third-party logistics (3PL) provider, or set up community pick-up points.
Here are some concrete steps to build an efficient delivery workflow:
- Map Participant Addresses: Use software to get a visual of all your delivery locations and plan the most efficient routes.
- Establish Communication Protocols: Set up a clear system—whether it’s text, email, or a phone call—to let participants know their delivery window. This one step can slash the number of missed deliveries.
- Develop Contingency Plans: Think ahead. Plan for the common hiccups like wrong addresses, no one being home, or a vehicle breakdown so you can solve problems fast.
- Track Delivery Data: Keep an eye on your metrics. On-time delivery rates and cost-per-delivery will help you constantly improve your operations and prove your efficiency to funders.
Measuring Program Success And Impact
To keep programs funded and show they're making a real difference, you have to prove it with clear, compelling data. For evidence-based nutrition interventions, this means going beyond feel-good stories to demonstrate measurable changes in people’s health and well-being. This section is a practical toolkit for measurement, designed to help you build a powerful case for funders and stakeholders.
The best place to start is with a solid logic model. It’s a simple tool that connects your program activities—like delivering weekly grocery boxes—to the short-term and long-term outcomes you’re aiming for. By mapping this out from the get-go, you can pick the right key performance indicators (KPIs) and health metrics to track.
Selecting Key Metrics And Outcomes
The metrics you choose have to match your specific intervention. A produce prescription program, for instance, will have entirely different success markers than a medically tailored meal program. It’s critical to track both process metrics (how well your program is running) and outcome metrics (the actual impact on participants).
- Process Metrics: These keep a finger on the pulse of your program's reach and fidelity. Think participant enrollment and retention rates, the number of meals or kits distributed, and on-time delivery percentages.
- Health Outcomes: This is where you measure direct health improvements. Common examples include changes in HbA1c for participants with diabetes, reductions in blood pressure, or shifts in food security scores (like those from the USDA survey module).
- Patient-Reported Outcomes: Don't forget the human side of the data. Surveys that capture changes in quality of life, stress levels, or a person’s confidence in managing their health condition add a rich, person-centered layer to your numbers.
Umoja Program Insight: We’ve learned that tracking program fidelity is just as important as measuring health outcomes. When we see high engagement rates and positive patient-reported feedback, it’s a strong leading indicator that our biometric data will also show improvement. It builds a complete picture of success.
The logistics of getting the food to people is the foundation of any good outcome. The infographic below shows the key steps that have to be tracked to make sure the program is delivered effectively.
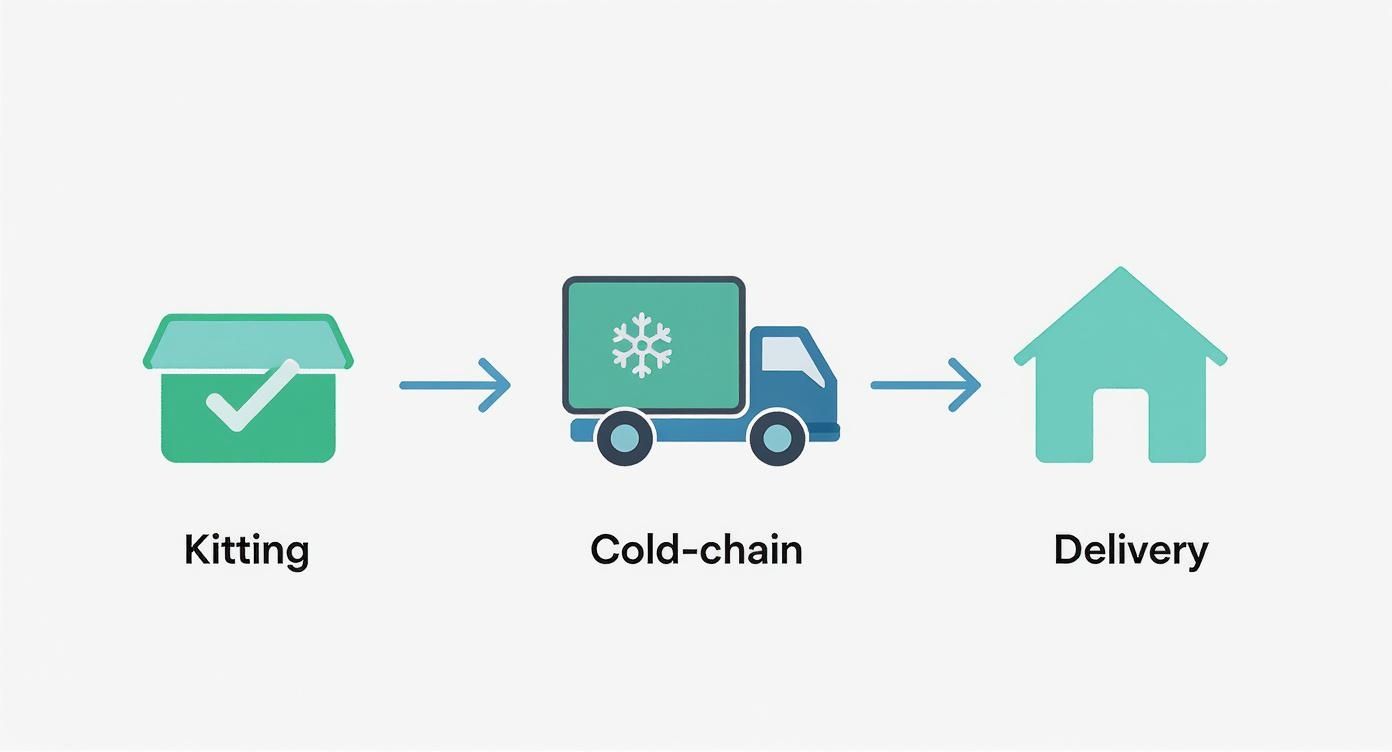
This just goes to show how operational success in kitting, cold-chain management, and delivery directly enables you to hit your health outcome goals.
The table below offers a simple template for aligning different intervention types with the right metrics.
Outcome Measurement Template For Nutrition Programs
| Intervention Type | Key Process Metric | Primary Health Outcome | Secondary Outcome |
|---|---|---|---|
| Medically Tailored Meals | Meal delivery adherence (%) | HbA1c reduction (for diabetes) | Reduced hospital readmissions |
| Produce Prescriptions | Voucher/box redemption rate (%) | Increased fruit/vegetable intake | Improved food security score |
| Behavioral Counseling | Session attendance rate | Weight loss (kg or % body weight) | Increased self-efficacy score |
| Senior Meal Kits (OAA) | Participant retention rate | Maintained nutritional status | Reduced social isolation |
By selecting metrics from each column, programs can build a balanced scorecard that tells the full story of their impact—from operational efficiency to life-changing health improvements.
Building A Data-Driven Case
Every data point you collect tells a story about your program’s value. Use this information to create reports that speak directly to what your funders care about, whether it's a health plan focused on cutting hospital readmissions or a foundation dedicated to improving community wellness. As you look at the bigger picture, new approaches like a data-driven longevity platform are also emerging, offering different ways to track the long-term effectiveness of these interventions.
By consistently tracking and reporting on a mix of operational, clinical, and patient-centered data, you can build a powerful, evidence-based case for continued investment and program expansion.
Making the Economic Case for Nutrition
To secure long-term funding, we have to frame evidence-based nutrition interventions as a high-return investment, not simply a cost. The economic data is clear: well-designed nutrition programs pay for themselves by slashing healthcare spending and boosting productivity. This shift in perspective is absolutely essential for building a powerful business case for policymakers, health systems, and funders.
Robust economic analyses consistently back this up. Programs like Medically Tailored Meals, for instance, have shown a 16% net reduction in healthcare costs. This savings comes mostly from preventing expensive hospital stays and emergency room visits. By keeping people healthier, these interventions relieve the massive financial strain chronic diseases put on the healthcare system.
Quantifying the Return on Investment
The economic benefits go far beyond direct healthcare savings. Better nutrition creates a healthier, more productive workforce and improves educational outcomes for kids, generating long-term value for society. This dual benefit—lower costs and higher productivity—makes nutrition an incredibly powerful investment.
The World Bank estimates that scaling up nutrition interventions to tackle undernutrition will require an extra $128 billion over the next decade. That sounds like a lot, but it’s dwarfed by the cost of doing nothing. Global productivity losses from overweight and obesity are pegged at $2 trillion annually, and the COVID-19 pandemic added another $29 billion in losses for 2023 alone. You can explore more about these global nutrition challenges and their economic impact to see the bigger picture.
Actionable Steps for Program Planners
To make a convincing economic argument, you need to present clear, data-driven projections. It’s about connecting the dots for funders.
- Focus on Cost Aversion: Frame your program's impact in terms of costs avoided. Calculate the potential savings from fewer hospital readmissions, a drop in emergency department visits, and better management of chronic diseases.
- Highlight Productivity Gains: Connect improved nutrition to real-world economic benefits. For adult programs, that could be fewer sick days. For child nutrition programs, link it directly to better school attendance and academic performance.
- Leverage Umoja's Insights: Our program evaluations consistently show that investing in culturally connected foods reduces waste and increases program adherence. This operational efficiency strengthens the financial case by maximizing the impact of every single dollar.
When you bring clinical outcomes and financial data together, you can prove that investing in evidence-based nutrition is more than just a moral imperative—it’s a fiscally sound strategy for building healthier, more prosperous communities.
Common Questions
This is where we get into the practical side of designing and implementing nutrition interventions that actually work. Here are some of the most common questions we hear from program planners and healthcare providers, with straightforward answers to help you navigate the tricky spots.
How Do We Choose the Right Intervention for Our Community?
There's no single "best" model; the right choice always starts with a deep look at your community's specific needs. A thorough needs assessment is non-negotiable. What are the demographics? What are the most common health challenges—diabetes, heart disease, food insecurity? And what resources are already on the ground?
For instance, if you're serving a population with high rates of diet-related chronic disease and many people have trouble getting around, Medically Tailored Meals might be the most direct route to impact. On the other hand, for communities in food deserts where people are eager to cook more, a Produce Prescription Program could be a perfect fit.
The key is to match the strongest evidence to your community’s unique profile. We've laid out the different models in our 'Core Categories of Nutrition Interventions' section—it's a great place to cross-reference and compare your options.
What Are the Biggest Hurdles in Securing Funding?
Funding is often the toughest part. The single biggest challenge is proving a clear return on investment (ROI) to potential funders like health plans or foundations. They need to see hard data on how your program will save them money down the line through reduced healthcare costs, fewer hospitalizations, and better health outcomes.
The best way to tackle this is to build a solid measurement plan from day one, which we detail in our 'Measuring Program Success and Impact' guide. Use pilot data from your own work and compelling evidence from established studies to project those potential savings.
Another common obstacle is the view that these programs are just "social services" instead of clinical care. You have to reframe the conversation. Presenting your work through the lens of 'Food as Medicine' helps align your goals directly with a funder's clinical and financial priorities.
How Can We Make These Models Culturally Appropriate?
Cultural adaptation isn't just a box to check; it’s absolutely critical for getting people to participate and stick with a program. The core evidence-based principles of an intervention should stay the same, but how you deliver it must be tailored to the community.
This means offering foods that people know and love, creating nutrition education in the right languages with relevant examples, and partnering with community leaders who are already trusted voices. For example, a produce prescription program can be transformed by sourcing vegetables from local farmers who grow culturally specific items.
Umoja Program Insight: We've seen a dramatic increase in program adherence when our nutrition kits feature culturally connected foods. Respecting and reflecting a community's dietary heritage isn't just a nice-to-have; it's a core component of an effective evidence-based nutrition intervention.
The most important rule? Always bring members of the target community into the design and feedback process. It’s the only way to ensure your program is truly relevant and respectful.
At Umoja Health, our expertise is helping organizations like yours design and scale compliant, effective, and culturally connected nutrition programs. Whether it's OAA-compliant senior kits or Food is Medicine grocery boxes, we handle the food, logistics, and know-how so you can focus on making a measurable impact. Learn how we can support your mission at umojahealth.com.