When we talk about heart-healthy meal programs, we're discussing structured dietary plans designed to seriously improve cardiovascular health. These aren't just about "eating healthy"—they're about providing specific meals low in sodium, unhealthy fats, and added sugars. Think of them as a cornerstone for managing conditions like hypertension and high cholesterol, built around nutrient-rich foods like fruits, vegetables, and lean proteins.
Common Meal Standards for Heart-Healthy Programs
Building an effective heart-healthy meal program starts with a rock-solid foundation of clinical and nutritional standards. This means we have to get much more specific than just telling people to "eat better." The real work is in defining measurable, evidence-based criteria that have a direct, positive impact on a person's health outcomes. Our goal is to create meals that are medically sound but also taste good enough that people will actually stick with the program long-term.
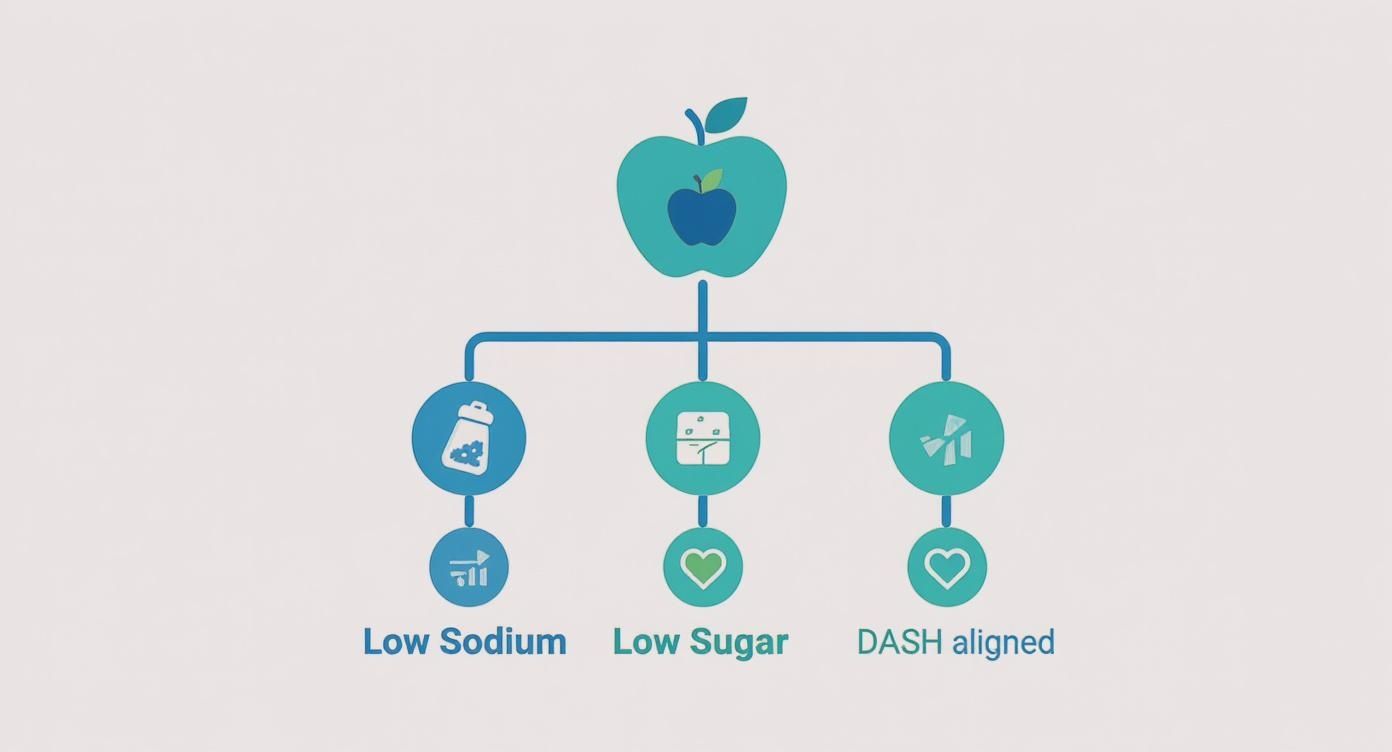
These standards are built on key nutritional pillars designed to fight the main drivers of cardiovascular disease. For any program to truly earn the "heart-healthy" label, its meals have to meet some very strict guidelines.
Core Nutritional Criteria
The most important standards are all about the specific nutrients that directly affect heart health. These are the non-negotiables:
- Sodium Limits: We know high sodium intake is a major cause of hypertension. A strong program will cap sodium at levels recommended by health authorities, which usually means around 600-800 mg per meal.
- Saturated and Trans Fat Restrictions: These are the fats that raise LDL ("bad") cholesterol, which in turn increases the risk of heart disease. Meals should get less than 10% of their total calories from saturated fat and have zero trans fats. Period.
- Controlled Sugar Content: Added sugars are a huge contributor to inflammation, weight gain, and poor metabolic health. Programs must limit them to help people maintain stable blood glucose levels and a healthy weight.
Adherence to these strict nutritional parameters is non-negotiable. It's the scientific basis that separates a genuinely therapeutic meal from a generally "healthy" one, forming the line between a wellness offering and a clinical intervention.
Evidence-Based Dietary Frameworks
These nutritional rules aren't created in a vacuum; they're often guided by established dietary patterns proven to support cardiovascular health. The Dietary Approaches to Stop Hypertension (DASH) diet is a perfect example and has become a global benchmark. It focuses on whole grains, fruits, vegetables, and lean proteins while limiting red meat, sweets, and sodium. The incredible success of the DASH diet really shows the power of a holistic, food-as-medicine approach.
If you want to go deeper on one of the most recommended dietary frameworks for heart health, it's worth understanding what a plant-based diet is and its core principles.
Adapting Standards for Diverse Populations
Let's be realistic: a one-size-fits-all approach almost never works. The best programs take these core principles and adapt them for different patient groups and cultural tastes. A patient just discharged from the hospital after a cardiac event needs something different than someone in a community wellness program. Even more importantly, ensuring meals feature familiar flavors and reflect a person's traditions is far more likely to be enjoyed and eaten consistently—which, at the end of the day, is the whole point.
Vendor Selection and Program Models
Picking the right operational model and vendor for a heart healthy meal program is a foundational decision that shapes everything from startup costs to quality of care. There’s no single "best" way to do it; the right structure depends on your organization’s resources and goals. Let's compare the common program models before diving into vendor selection.
Comparing Heart-Healthy Program Models
- In-House Production: This model, often used by large hospitals, offers maximum control over menus and quality but requires significant upfront investment in kitchen infrastructure, staff, and regulatory compliance. It's best for large-scale operations with existing kitchens and a need for highly specialized medical diets.
- Food Vendor Partnership: Outsourcing meal production to a specialized company is a popular route that slashes capital costs and operational complexity. This frees you to focus on patient care, but it requires rigorous vetting to ensure the partner consistently meets your nutritional and cultural standards.
- Community Kitchen Collaboration: This hybrid approach leverages shared resources with local non-profits, offering a cost-effective, mission-aligned solution for smaller organizations or pilot programs. The main challenge is ensuring consistent quality and scalability.
This table evaluates the three common meal program models based on key operational and strategic criteria.
| Criterion | In-House Production Model | Food Vendor Partnership Model | Community Kitchen Model |
|---|---|---|---|
| Upfront Cost | Very High (equipment, space, staffing) | Low to Moderate (setup fees, initial order) | Low (leverages existing infrastructure) |
| Operational Control | Maximum (full control over menu, sourcing, QA) | Moderate (set standards, vendor executes) | Variable (depends on partnership agreement) |
| Scalability | High (limited only by your infrastructure) | Very High (vendor handles production increases) | Limited (often constrained by partner's capacity) |
| Speed to Launch | Slow (requires significant planning, setup) | Fast (can launch in weeks to months) | Moderate (depends on partner readiness) |
| Staffing Needs | High (kitchen staff, dietitians, logistics) | Low (focus on program management, enrollment) | Moderate (liaison, some shared staff) |
| Best For | Large health systems with existing kitchens | Orgs wanting to focus on care, not cooking | Small CBOs, pilot programs, budget-conscious |
How to Select the Right Meal Program Vendor
When you decide to bring in an external partner, you're placing a huge amount of trust in their hands. Choosing the right vendor means looking way beyond the menu and the price tag.
Your core standards should always include:
- Food Safety and Certifications: The vendor must hold current, relevant food safety certifications, like HACCP or SQF.
- Nutritional Guideline Adherence: They have to show—not just tell—that they can consistently hit your specific heart-healthy nutritional targets. Ask for sample menus with detailed nutritional analyses.
- Ingredient Sourcing and Transparency: Ask about their procurement policies. Sourcing transparency is a huge tell for a quality-focused operation.
- Cultural Competency: A vendor's ability to produce culturally connected meals is not a "nice-to-have" feature; it is a core component of patient adherence and program effectiveness.
A critical piece to examine is their packaging and delivery logistics. If your goal is to streamline distribution and maintain brand consistency, understanding a vendor's process here is vital. You can get a better sense of how a partner can support your branding with our guide to private label packaging setup.
Patient Communication and Program Adoption
Great food is only half the battle in heart healthy meal programs. What really drives long-term health improvements is sustained patient engagement. When you get communication right, a simple meal delivery transforms into a supportive, empowering experience. A structured implementation plan ensures this communication is woven in from the start.

Umoja Health’s Program Adoption Steps: A Framework
Moving a program from concept to operation requires a clear plan. At Umoja Health, we use a straightforward process to help organizations launch successful programs, integrating patient communication at every step.
- Goal Alignment: We sit down with you to understand your patient population, clinical goals, and budget. This defines the "why" and sets measurable targets, like reducing hospital readmissions.
- Menu Curation & Workflow Design: We work with your team to design culturally connected, 12-week grocery programs that meet strict heart-healthy standards. Simultaneously, we map the entire participant journey, from a simple enrollment process to automated delivery notifications. For individuals, success often comes down to mastering practical meal prepping techniques, and a program's workflow should be just as straightforward.
- Logistics and Kitting: We manage all procurement, kitting, and nationwide delivery of shelf-stable food boxes directly to participants' homes. This phase is governed by robust Standard Operating Procedures (SOPs) that ensure quality and consistency. Our experience with compliant kitting programs is key here.
- Reporting and Feedback: We provide tools to track metrics and establish a feedback loop. This allows you to demonstrate ROI to stakeholders while continuously improving the program based on participant input.

Boosting Engagement with Effective Communication
A solid communication plan isn't an afterthought. It starts from day one and continues throughout the participant's entire journey.
- Onboarding: The onboarding process sets the tone. A clear, welcoming introduction via a welcome kit and a personal call can make a huge difference in getting initial buy-in.
- Education and Support: Beyond meals, provide educational materials that reinforce the "why." Simple recipe cards, infographics on reading nutrition labels, or tips for cutting sodium empower participants to take an active role in their health.
- Feedback Collection: Systematically collecting feedback on meal quality and delivery experience is a core operational requirement. Use simple surveys and follow-up calls to gather insights, then use that data to make tangible improvements.
Consistent, supportive communication is the bridge between providing healthy food and achieving lasting behavior change. It ensures participants feel like active partners in their own health journey, not just passive recipients of a service.
Measuring Program Success and Proving ROI
To keep your heart healthy meal programs funded and growing, you have to prove they work. This means quantifying your impact in a way that resonates with stakeholders. Building a solid measurement strategy isn't just about tracking metrics; it's about telling a powerful story of better health and a real return on investment (ROI).
Key metrics to keep your eye on:
- Clinical Outcomes: Track changes in biometric markers like blood pressure, A1c levels, and cholesterol. Seeing these numbers drop provides direct evidence of improved cardiovascular health.
- Operational Metrics: Measure program adherence rates, participant satisfaction scores, and delivery accuracy. High marks here show the program is running efficiently.
- Financial Indicators: Calculate the reduction in hospital readmission rates, fewer emergency room visits, and the lower overall healthcare costs for your participants.
The most compelling ROI story combines hard data with human experience. A testimonial from a participant describing how they have more energy to play with their grandkids can be just as powerful as a chart showing a 10% reduction in hypertension.
Your data has to be presented in a way that grabs your audience. The concept of ROI in nutrition programs is well-established. According to the Global Survey of School Meal Programs, for every dollar invested, these programs create up to $35 in economic and social benefits. This proves that investing in heart healthy meal programs isn't just an expense—it's a strategic investment in a community's well-being with a significant, proven return.
Here are a few common questions we hear from program managers on the ground.
How Can We Keep Program Costs in Check Without Sacrificing Quality?
This is the big one, isn't it? Managing a budget while delivering high-quality meals is always top of mind. One of the most effective strategies we've seen is building menus around shelf-stable ingredients. This move dramatically cuts down on food waste and untangles a lot of logistical knots.
Another key is partnering with a vendor who lives and breathes bulk procurement. They can lock in better pricing on quality, compliant foods. Also, think seasonally. Designing menus around produce that's in season, alongside cost-effective proteins like beans and legumes, keeps costs down. These ingredients aren't just budget-friendly; they're the foundation of proven heart-healthy diets like the DASH framework.
What’s the Best Way to Handle Diverse Dietary Needs?
Successfully serving a diverse community starts long before the first meal is packed. It begins with a thoughtful participant intake process. You need to collect detailed information on allergies, cultural preferences, and specific medical needs right from the start.
From there, work with a partner who can provide customizable meal components or, even better, create truly culturally connected menus. It makes a world of difference when you can offer Latin-inspired, Asian, or Soul Food-style heart-healthy options. Meals need to be more than just clinically sound—they need to be genuinely appealing to the people eating them. That’s how you drive real adherence.
A common mistake is treating cultural adaptation as an afterthought. To ensure participant buy-in, culturally relevant meals must be a core part of the program's design from day one, not a special exception.
How Do We Get Patients to Stick with the Program?
Boosting adherence is about more than just the food; it's about building a supportive, communicative relationship. A structured onboarding process is critical for setting clear expectations and establishing trust right out of the gate.
Then, you have to keep listening. Regularly collect participant feedback, whether through simple surveys or quick check-in calls. When people feel heard and see their suggestions lead to actual changes—like a new item on the menu—they become invested. That feedback loop is the engine that maintains engagement and ultimately drives better health outcomes.
Ready to launch a compliant, culturally connected, and effective heart-healthy meal program? Umoja Health provides the expertise and logistical support to deliver nutritious food boxes nationwide, helping you achieve measurable outcomes for your community. Learn more at https://umojahealth.com.

