Telling a patient with high blood pressure to just "eat better" is a recipe for failure. It's vague advice that rarely sticks because it lacks a clear plan and real-world support. This is where effective hypertension nutrition programs come in. They move past generic recommendations and offer structured interventions—things like personalized menu planning, practical sodium monitoring, targeted patient education, and consistent digital engagement that actually drives lasting health improvements. It turns a fuzzy suggestion into a concrete, supported lifestyle change.
Why Most Hypertension Diets Fail Patients

Handing someone a one-size-fits-all diet sheet ignores the messy reality of their life. It doesn't account for cultural food preferences, tight budgets, or just plain busy schedules. Without a clear, supportive framework, patients are left to sort through a sea of conflicting information online, which almost always leads to frustration and giving up.
This is exactly the gap that a well-designed hypertension nutrition program fills. These programs aren't about restriction; they’re about empowerment. By providing tangible tools and step-by-step guidance, they help people build habits that stick. It’s an approach that understands managing high blood pressure is a marathon, not a sprint.
Core Interventions of a Successful Program
A truly impactful program isn’t just one thing—it’s a combination of key supports that address the different facets of managing hypertension. When these interventions work together, they create a powerful support system for the patient.
- Culturally-Aware Menu Planning: A diet plan only works if someone is willing to follow it. Success hinges on creating menus that respect and include a person's cultural background, making healthy eating feel familiar and natural, not like a punishment.
- Proactive Sodium Monitoring: Simply saying "cut back on salt" isn't enough. Good programs teach people how to do it—how to read labels, spot hidden sodium in processed foods, and make smarter choices at the grocery store.
- Targeted Patient Education: Knowledge is power. Education modules that break down complex health topics into simple, actionable steps give patients the confidence to take control of their own health.
- Consistent Digital Engagement: Modern programs use simple digital tools to provide ongoing support. This could be anything from automated text reminders to direct messaging with dietitians, making sure patients feel connected and accountable.
A well-designed nutrition program bridges the gap between a doctor's recommendation and what a person actually does every day. It’s built on a foundation of personalization, practical education, and consistent support.
From Theory to Impactful Outcomes
Partners like Umoja have shown how these structured programs can drive real, measurable improvements. By implementing these core interventions, we see tangible drops in blood pressure and, as a result, lower healthcare costs. For example, by delivering medically tailored groceries and educational resources right to people's doors, one Umoja-supported program saw a 12-point average reduction in systolic blood pressure among participants. This model proves that a thoughtful, evidence-based program is one of the most powerful tools we have for managing chronic disease. To see more strategies behind successful health initiatives, you can check out our insights on thought leadership in healthcare.
The most scientifically validated approach, the Dietary Approaches to Stop Hypertension (DASH) diet, continues to be the gold standard worldwide. It was developed with support from the U.S. National Heart, Lung, and Blood Institute and was recently named the number one 'Best Heart-Healthy Diet' by U.S. News & World Report. That kind of recognition underscores just how powerful a structured, food-first approach can be.
Alright, let's get into the nuts and bolts of building a hypertension nutrition program that actually works. It's one thing to have the right intentions, but you need a solid blueprint to see real, lasting results for your members.
Building Your Program From the Ground Up

From my experience, the most effective programs are built on four core intervention areas that support patients from every possible angle. These aren't just separate tactics; they're interconnected pillars that create a complete support system.
When you thoughtfully weave these pieces together, you turn a complex medical directive—"lower your blood pressure"—into a series of clear, manageable actions patients can take every single day.
Let’s take a look at the core components of a program that drives real change. The table below breaks down the four key pillars, the specific actions you need to take, and the tools that make it all happen.
Core Components of a Hypertension Nutrition Program
| Intervention Pillar | Key Actions & Strategies | Tools & Resources |
|---|---|---|
| Strategic Menu Planning | – Develop culturally relevant menus. – Offer medically tailored meal kits. – Adapt traditional recipes to be low-sodium. |
– Patient preference surveys – Registered Dietitian (RD) consultations – Pre-portioned meal kits and recipe cards |
| Practical Sodium Monitoring | – Teach practical label-reading skills. – Provide visual guides for sodium content. – Use simple food swap comparisons. |
– Nutrition Facts label guides – Infographics (the "Salty Six") – Low-sodium shopping lists |
| Impactful Patient Education | – Create interactive, hands-on learning. – Simplify complex concepts with analogies. – Use cooking demos to teach flavor building. |
– "Scavenger hunt" activities – Live or virtual cooking classes – Tip sheets on using herbs and spices |
| Smart Digital Engagement | – Send automated reminders and prompts. – Offer simple progress-tracking dashboards. – Provide direct access to dietitians. |
– SMS/text messaging platforms – Simple mobile apps with tracking features – Secure messaging portals for Q&A |
By focusing your efforts on these four areas, you create a program that's not just informative but truly empowering. Now, let’s dig into how you can bring each one to life.
Intervention 1: Strategic and Culturally Relevant Menu Planning
A meal plan is useless if it ends up in the trash. The foundation of a successful nutrition program is a menu that people will actually eat and enjoy. This means moving beyond generic DASH diet flyers and creating plans that resonate with individual lives.
For instance, suggesting grilled chicken and steamed broccoli might not land well with a family accustomed to Latin American cuisine. A better fit? A low-sodium black bean and corn salsa with baked plantains and grilled fish. The nutritional goals are identical, but the cultural connection makes all the difference.
Umoja’s Step-by-Step Implementation:
- Patient Intake: We start with detailed surveys to understand a person's cultural background, food preferences, allergies, and kitchen confidence. This data forms the basis of a truly personalized plan.
- Recipe Adaptation: Our dietitians adapt beloved traditional recipes to meet strict sodium guidelines without sacrificing flavor. This shows respect for their culture and increases the likelihood of adherence.
- Medically Tailored Meal Kits: We build weekly meal kits with pre-portioned, compliant ingredients and simple, visual recipe cards. This removes the guesswork and decision fatigue, making healthy cooking feel achievable.
This approach transforms the meal from a medical chore into a positive, familiar experience—the key to long-term adherence and improved health outcomes.
Intervention 2: Practical Sodium Monitoring
Telling a patient to eat less than 1,500 mg of sodium a day is just an abstract number. To make that real, you have to give them simple, practical ways to track it. The goal is to demystify sodium and empower them to make smart choices on their own.
Your education must be laser-focused on label literacy. Create simple visual guides that show them exactly where to look on a Nutrition Facts panel and what to look for: the milligrams of sodium and the % Daily Value (%DV).
Umoja’s Step-by-Step Implementation:
- Visual Education: We provide simple infographics that highlight the "Salty Six"—common high-sodium foods like bread, deli meats, and pizza—so patients know where sodium hides.
- Skill-Building Workshops: We run virtual workshops teaching patients how to read labels, compare products at the grocery store, and make smart, low-sodium swaps.
- Practical Tools: We include low-sodium shopping lists and recipe cards that explicitly state the sodium content per serving, making it easy for patients to track their daily intake without complex calculations.
This practical focus turns an overwhelming task into a manageable skill, leading to sustained behavior change.
Intervention 3: Impactful Patient Education
The best education makes complicated things feel simple and gives people clear actions to take. A module on reading food labels, for example, shouldn't be a dry lecture. It needs to be a hands-on workshop.
Umoja’s Step-by-Step Implementation:
- Bite-Sized Learning: We deliver educational content through multiple channels—text messages, short videos, and simple tip sheets included in meal kits. We might focus one week on "Flavoring with Herbs" and the next on "Decoding Drink Labels."
- Interactive Activities: We create challenges like a "Label Scavenger Hunt," encouraging patients to find the lowest-sodium option for a common food item at their local store and share their findings.
- Cooking Demos: We provide access to live or pre-recorded cooking demos that show how to build flavor with spices, citrus, and garlic instead of relying on salt, making the lessons tangible and delicious.
These interactive methods make the information stick and ensure that lessons learned translate into behavior change at home, driving positive case outcomes like improved blood pressure control.
Intervention 4: Smart Digital Engagement
In our work at Umoja, we've seen how digital tools can be a game-changer. Technology helps maintain a supportive, consistent connection with patients between formal appointments, boosting accountability and motivation.
We're not talking about complicated apps. Simple, accessible digital touchpoints can make a massive difference.
Umoja’s Step-by-Step Implementation:
- Automated Nudges: Simple SMS text messages prompt patients to log their meals, check their blood pressure, or offer a quick tip for the day. This keeps the program top-of-mind.
- Progress Tracking: A clean digital dashboard lets patients see their blood pressure readings trend down over time. Seeing their own success is powerful positive reinforcement.
- Direct Dietitian Access: We provide a secure messaging platform for patients to ask a registered dietitian a quick question. This immediate support can prevent small doubts from derailing their progress.
When you bring these four interventions together—thoughtful menus, practical sodium tracking, engaging education, and supportive digital tools—you build a robust hypertension nutrition program that empowers people to take control of their health.
Solving the Patient Adherence Puzzle

Let's be honest. You can design the most perfect, evidence-based hypertension nutrition program in the world, but it's useless if patients don't stick with it. Adherence is the single biggest hurdle we face, and it's where even the best plans fall apart.
The first step is understanding why people struggle. The reasons are always complex and deeply personal, ranging from food insecurity to the simple motivational dips we all experience. To really solve this puzzle, we have to move past just identifying problems and start implementing a toolkit of solutions that meet these challenges head-on.
It's all about making a daunting lifestyle overhaul feel like a series of small, achievable wins. This means personalizing the plan to fit real lives, providing support that's always within reach, and using a little behavioral science to help build habits that last.
Personalized Menu Planning Meets Real Life
The core of adherence is enjoyment. If a meal plan feels like a punishment, it won't last a week. We've seen firsthand at Umoja that personalizing menus to a patient’s cultural background and personal tastes is non-negotiable.
For instance, instead of handing over a generic low-sodium PDF, we might work with someone to create a heart-healthy version of their family’s favorite stew. This simple act of adapting familiar foods makes the whole process feel less clinical and more collaborative. It acknowledges that food is more than just fuel; it's comfort and identity.
A key insight from our work is that success comes from meeting patients where they are. We don’t force them into a rigid, unfamiliar diet. Instead, we co-create a plan that respects their traditions and preferences, which dramatically boosts their engagement and commitment.
Making Sodium Monitoring an Achievable Habit
Telling someone to track their sodium intake is easy. Actually teaching them how to do it consistently is the real work. The most effective programs use simple, visual tools that make this abstract goal concrete and manageable.
We focus on practical skills like "sodium budgeting." We might show a patient that their favorite canned soup uses up 60% of their daily sodium allowance. Framing it this way helps them see their intake as a finite resource, empowering them to make smarter trade-offs throughout the day.
This approach is critical. Despite the proven benefits of diets like DASH, adherence is a huge issue. Data from the National Health and Nutrition Examination Survey (NHANES) showed that people with hypertension often find it harder to follow DASH guidelines than those without the condition. It's a clear gap between knowing and doing. You can dig into more on this in the CDC’s findings on dietary adherence.
Education That Empowers, Not Overwhelms
Patient education has to be simple, consistent, and immediately useful. We've found that breaking down complex information into bite-sized, actionable tips—delivered through multiple channels—is far more effective than a single, lengthy onboarding session.
Here’s how we structure our educational outreach for maximum impact:
- Weekly Themed Content: We'll focus on just one topic each week, like "Decoding Food Labels" or "Flavoring with Herbs, Not Salt." This prevents information overload.
- Hands-On Activities: We might send a "label scavenger hunt" challenge via text, asking patients to find the lowest-sodium bread at their local grocery store.
- Quick Reference Guides: Simple infographics or wallet cards summarizing key concepts, like the "Salty Six" foods to watch out for, serve as easy reminders right when they're needed.
This steady stream of simplified communication keeps patients engaged and reinforces key lessons without feeling like a chore.
Digital Engagement for Continuous Support
Technology can be a vital lifeline, offering support and accountability between formal check-ins. The goal isn't to add complexity but to make support more accessible and timely.
We've learned that simple tools often drive the best results. A secure messaging portal allows a patient to ask a dietitian a quick question while they're in the grocery aisle. Automated SMS reminders can prompt them to log a blood pressure reading or prep a healthy meal.
These small digital touchpoints create a sense of constant, low-pressure support. They help patients build momentum and feel connected to their care team, turning what can feel like a lonely struggle into a guided partnership. It's this combination—personalization, practical education, and consistent engagement—that truly cracks the adherence puzzle.
When we're designing nutrition programs for hypertension, the conversation usually starts and ends with sodium and fat. But to build something truly effective, we need to go deeper. There's a new frontier in blood pressure management, and it's all happening inside our gut.
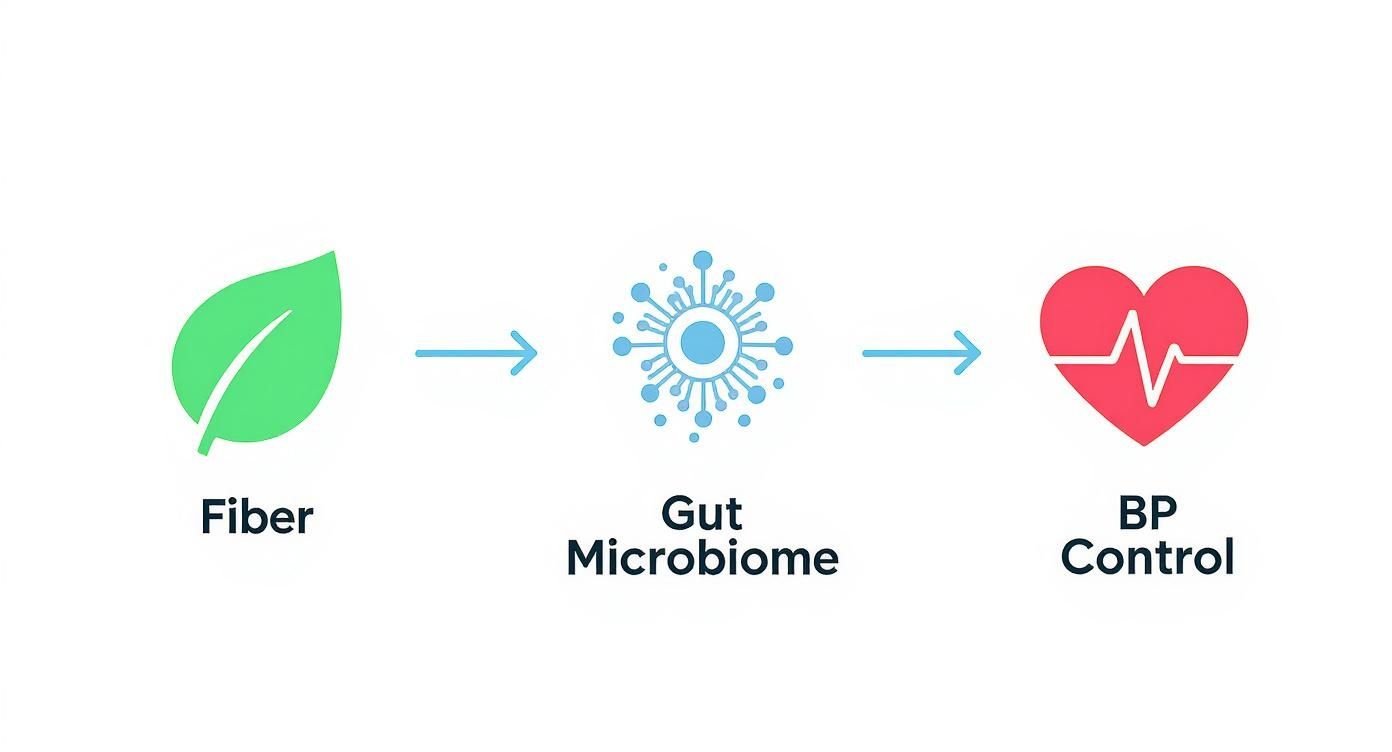
The link between our gut microbiome—those trillions of bacteria living in our digestive tract—and cardiovascular health is becoming impossible to ignore. It offers a powerful new angle for any dietary intervention.
This is about so much more than just digestion. The bacteria in our gut are tiny powerhouses, helping to regulate inflammation, produce hormones, and even control how our blood vessels function. When this delicate ecosystem gets out of balance (a state called dysbiosis), it's directly linked to higher blood pressure. The great news? We can influence this balance with the food we eat, making it a critical strategy for any modern nutrition program.
The Gut-Blood Pressure Connection
So, how exactly does this work? It’s pretty fascinating.
Healthy gut bacteria thrive on specific foods, especially fiber. When they consume this fiber, they produce beneficial compounds called short-chain fatty acids (SCFAs). These SCFAs get into the bloodstream and work their magic by helping to relax blood vessels and reduce inflammation, which ultimately helps lower blood pressure.
On the flip side, a diet low in these key nutrients allows harmful bacteria to take over, creating an environment that actually promotes hypertension. By simply shifting the diet to feed the good microbes, we can kickstart a positive feedback loop that supports cardiovascular health from the inside out.
The science is there. A recent study found that for every one-unit increase in a dietary index geared toward a healthy gut, there was a 4% reduction in hypertension risk. That’s a direct, measurable connection. You can dig into the findings to understand how diet impacts gut health and hypertension risk.
Actionable Strategies for Menu Planning
Folding gut health into your program doesn't mean you have to scrap everything and start over. It's about making strategic additions—foods that act as fuel for those beneficial bacteria. The focus should be on diversity and nutrient density.
- Prioritize Prebiotic-Rich Foods: These are the five-star meals for good gut bacteria. Think garlic, onions, asparagus, bananas, and whole grains like oats and barley. They're surprisingly easy to weave into almost any meal plan.
- Increase Soluble Fiber: Foods like beans, lentils, apples, and carrots are loaded with soluble fiber, a favorite food for producing those all-important SCFAs. A simple black bean and corn salsa, for example, is a fantastic, fiber-packed addition to a meal.
- Emphasize Polyphenols: Found in brightly colored fruits and vegetables like berries and dark leafy greens (and even dark chocolate!), these compounds have antioxidant effects and help create a healthy gut environment.
A gut-healthy diet isn't about restriction; it's about intentional addition. By focusing on adding fiber, prebiotics, and a variety of colorful plants, you naturally crowd out the processed foods that can harm both gut balance and blood pressure.
For those wanting to take a structured deep dive, something like a 30-day gut healing diet plan guide can provide an excellent framework.
Putting It All Together for Superior Outcomes
When you start weaving these principles into your menu planning, you create a much more holistic and powerful intervention.
Imagine a medically tailored meal kit that includes whole-grain quinoa, black beans, and a side of steamed asparagus. That single meal is rich in both fiber and prebiotics. This approach doesn't just check the boxes for traditional hypertension goals; it actively nurtures the gut microbiome for a compounded, lasting effect.
This focus on the gut is what will set your hypertension nutrition program apart. It goes beyond the standard advice and gives patients an advanced, science-backed strategy for long-term health. Of course, the best plan in the world only works if people can get the food, which is why consistent access is so crucial. It’s a challenge we’re committed to solving through our work in promoting nutrition security.
Your Implementation and Logistics Blueprint
https://www.youtube.com/embed/MrsOZLNddfI
An idea for a program is only as good as its execution. This is where you roll up your sleeves and build the operational blueprint that turns a well-designed hypertension nutrition program from a concept into a reality for patients. This is the backbone that ensures the right food gets to the right people, safely and on time.
From our direct experience at Umoja, a successful operational model rests on a few key pillars: meticulous vendor selection, ironclad food safety protocols, and a seamless, welcoming patient onboarding process. When these pieces click into place, you create an efficient, scalable infrastructure that can actually deliver consistent, life-changing results.
Sourcing and Procurement Best Practices
The quality of your program literally starts with the ingredients you source. For medically tailored meals targeting hypertension, this means finding suppliers who can meet incredibly strict low-sodium and nutritional compliance standards. This isn't just a suggestion; it's the foundation of patient safety and program efficacy.
When vetting potential vendors, your checklist needs to be rigorous. Don't just accept general statements—ask for detailed nutritional data for every single product. It’s also vital to dig into their supply chain reliability, especially for fresh produce, to head off any disruptions that could throw your patients' meal plans into chaos.
Here’s a practical look at what to prioritize:
- Supplier Vetting: Require comprehensive nutritional specs and complete allergen information for all ingredients. No exceptions.
- Quality Control: Set up clear protocols for receiving and inspecting goods to ensure they meet your standards with every delivery.
- Scalability: Partner with suppliers who can grow with you. You need to know they can maintain quality and consistency as you serve more people.
Your procurement process is the program's first line of defense. A partnership with a reliable, transparent supplier is the bedrock of a safe and effective hypertension nutrition program. It prevents a cascade of downstream issues with compliance and quality.
Managing Logistics and Third-Party Partners (3PL)
Once you have the right ingredients, the next puzzle is getting them from your facility to your patients' doorsteps. For many organizations, the most efficient route is partnering with a Third-Party Logistics (3PL) provider to handle the heavy lifting of storage, kitting, and delivery. A great 3PL partner doesn't just move boxes; they become a true extension of your team.
Look for a 3PL with specific, verifiable experience in handling food-grade products. They absolutely must be FDA-registered and fluent in the complexities of allergen-segregated storage and cold-chain management. These aren't just details; they are non-negotiable for ensuring food safety from the warehouse to the front door. For a deeper dive into how these partnerships function, check out our guide on specialized kitting programs that live and die by precise logistics.
Technology is your best friend here. A modern 3PL should offer a robust Warehouse Management System (WMS) that gives you real-time visibility into inventory, order status, and delivery tracking. This data is invaluable for managing your program efficiently and spotting potential issues before they ever impact a patient.
The diagram below shows how something as simple as dietary fiber can positively influence the gut microbiome, which in turn helps support better blood pressure control.
This really gets to the heart of the logistical challenge: you're delivering foods with specific, functional benefits that support the program's clinical goals from the inside out.
Designing a Seamless Patient Onboarding Experience
The final piece of the logistics puzzle is all about the patient. A smooth onboarding experience sets the tone for the entire program and can make or break long-term adherence. That first touchpoint—whether it's an online form or a phone call—has to be simple, clear, and reassuring.
Gather the essential information without making it feel like an interrogation. You'll need delivery details, dietary restrictions, and how they prefer to be contacted. Use this info to create a personalized welcome kit. This shouldn't just be their first box of meals; include simple, easy-to-read materials that explain how the program works and what to expect.
Clear communication is everything. Patients need to know exactly when their deliveries are coming and who to call with questions. Simple tools like automated SMS notifications can provide delivery updates and serve as gentle reminders, keeping them engaged and feeling supported from day one.
Of course. Here is the rewritten section, designed to match the expert, human-written style of the provided examples.
Your Hypertension Program Questions, Answered
When you're in the trenches designing and running a hypertension nutrition program, the same questions tend to pop up. You’re juggling patient care, complex logistics, and new technology. Getting clear, straightforward answers is critical. Here’s our take on some of the most common queries we hear.
How Do You Really Know if the Program Is Working?
Measuring the success of a hypertension program isn’t about a single number. The true impact is a blend of clinical outcomes, how engaged your patients are, and whether the whole thing runs smoothly. You need the complete picture to see what's clicking and where you can improve.
Obviously, the primary clinical indicators are lower systolic and diastolic blood pressure readings. We also look for improvements in related biomarkers, like LDL cholesterol. But these numbers only tell part of the story.
Just as important is patient engagement. We track this through program retention rates and patient satisfaction surveys. Are people sticking with it? Do they feel supported and empowered? High engagement is a huge predictor of long-term clinical success.
Finally, we look at operational metrics like on-time delivery rates and overall cost-effectiveness. This ensures the program is not just effective, but also sustainable and reliable for the people who depend on it.
A comprehensive dashboard that pulls together these three areas—clinical, engagement, and operational metrics—is the only way to see the full story of your program's impact. It lets you demonstrate value not just in health outcomes, but in member satisfaction and logistical excellence.
What Are the Biggest Headaches in Sourcing Food?
For medically tailored meals, getting the food sourcing right is one of the biggest operational hurdles. The challenges really boil down to three things: guaranteeing strict ingredient compliance, managing costs, and locking in consistent quality and availability.
The toughest part is ensuring every single component meets specific nutritional guidelines, especially for low-sodium diets. This demands thoroughly vetted suppliers who can provide detailed nutritional data and stick to rigorous food safety protocols. It's not enough for a supplier to just say an ingredient is "low sodium"; you need verifiable data to prove it.
Supply chain reliability, particularly for fresh produce, is another major concern. We’ve found that building strong, transparent relationships with suppliers and having strict internal quality control checks are essential for getting ahead of these issues. This kind of proactive approach stops compliance problems before they can ever reach a patient's plate.
How Can We Use Technology to Keep Patients Engaged?
Technology can be a game-changer for boosting engagement in a hypertension nutrition program. When used thoughtfully, it makes patients feel more connected, supported, and motivated. The key is to use simple, accessible tools that make things easier for them, not more complicated.
A few things we’ve seen work well:
- Mobile Apps for Motivation: A simple app can send daily meal reminders, share bite-sized educational content, and let patients track their own progress. There's nothing more motivating than seeing your own blood pressure numbers trend downward.
- Digital Platforms for Support: Secure messaging portals connecting patients directly with registered dietitians are invaluable. They can get quick, personalized answers to questions that might otherwise derail their progress.
- Gamification for Habit Building: Incorporating simple gamification—like earning badges for consistently logging meals or hitting activity goals—can make the process more enjoyable and help build lasting habits.
Telehealth consultations also play a huge role by removing travel barriers and making it easier for patients to get the professional guidance they need. By making the program more interactive and accessible, technology helps turn a passive experience into an active partnership in their health.
At Umoja Health, we build and support hypertension nutrition programs that deliver measurable results by focusing on these core principles. To learn how we can help you design and launch a compliant, culturally relevant program, visit umojahealth.com.