Let's get straight to the point: a community's health begins with its mothers. Maternal nutrition programs are more than just a public health initiative; they are a direct line to healthier babies, stronger families, and thriving communities. These programs provide essential food, education, and resources to women during pregnancy and in the first months after birth, directly shaping birth weights, brain development, and long-term health.
Why Maternal Nutrition Programs Are a Must-Have
Good nutrition during the perinatal period isn't just about "eating for two." It's one of the most powerful investments we can make in the future. When new and expectant mothers get the nutrients they need, the positive effects ripple outward. These programs are not simply handing out food; they are a core strategy for breaking generational cycles of poor health and inequality.
The science on this is settled. What a mother eats directly builds the foundation for her child's life. Poor nutrition can lead to low birth weight, developmental delays, and a higher risk for chronic diseases down the road. On the flip side, targeted nutritional support paves the way for healthier pregnancies, stronger babies, and more resilient families.
The Global and Local Impact
This isn't a new idea, but it's gaining urgency. Recognizing the critical window of opportunity, UNICEF launched its Improving Maternal Nutrition Acceleration Plan in 2023. The goal is massive: reach 16 million women and girls across 16 countries by 2025 with a full suite of services, from education to micronutrient supplements. This is about decisively breaking the cycle of poverty and poor health on a global scale.
Here at home, these programs are a vital safety net. They work to ensure every mother, no matter her zip code or income, has the building blocks for a healthy pregnancy. This is the heart of nutrition security, where everyone has consistent access to the food they need to flourish.
By closing nutrient gaps and offering steady support, maternal nutrition programs are one of our best tools for reducing birth complications and promoting healthy fetal growth. It's a proactive approach that doesn't just save on healthcare costs—it saves lives.
Beyond Pregnancy: A Lifelong Connection
The benefits don't stop at delivery. A well-nourished mother is better prepared for the physical demands of recovery and the marathon of caring for a newborn. Good nutrition also supports mental well-being during a vulnerable time. And, importantly, it underscores the critical link between maternal nutrition and breastfeeding.
Ultimately, these programs deliver more than just groceries. They provide education, build community connections, and empower women with the confidence and knowledge to make healthy choices for themselves and their children. They are an indispensable part of public health, laying a stronger, healthier foundation for the next generation.
How to Run a High-Impact Maternal Nutrition Program
Getting a prenatal and postpartum nutrition program off the ground means building a solid operational blueprint, from picking a delivery model to locking down sustainable funding. The structure you choose has to fit your community’s specific needs, your team's capabilities, and your budget. Real success comes from creating a practical framework that reliably gets nourishing food to mothers and their children.
This isn't just about logistics; it's about breaking a cycle. As the visual below shows, the impact is powerful and direct—a well-run program can set a child up for a healthy future, while its absence can perpetuate a cycle of malnutrition.
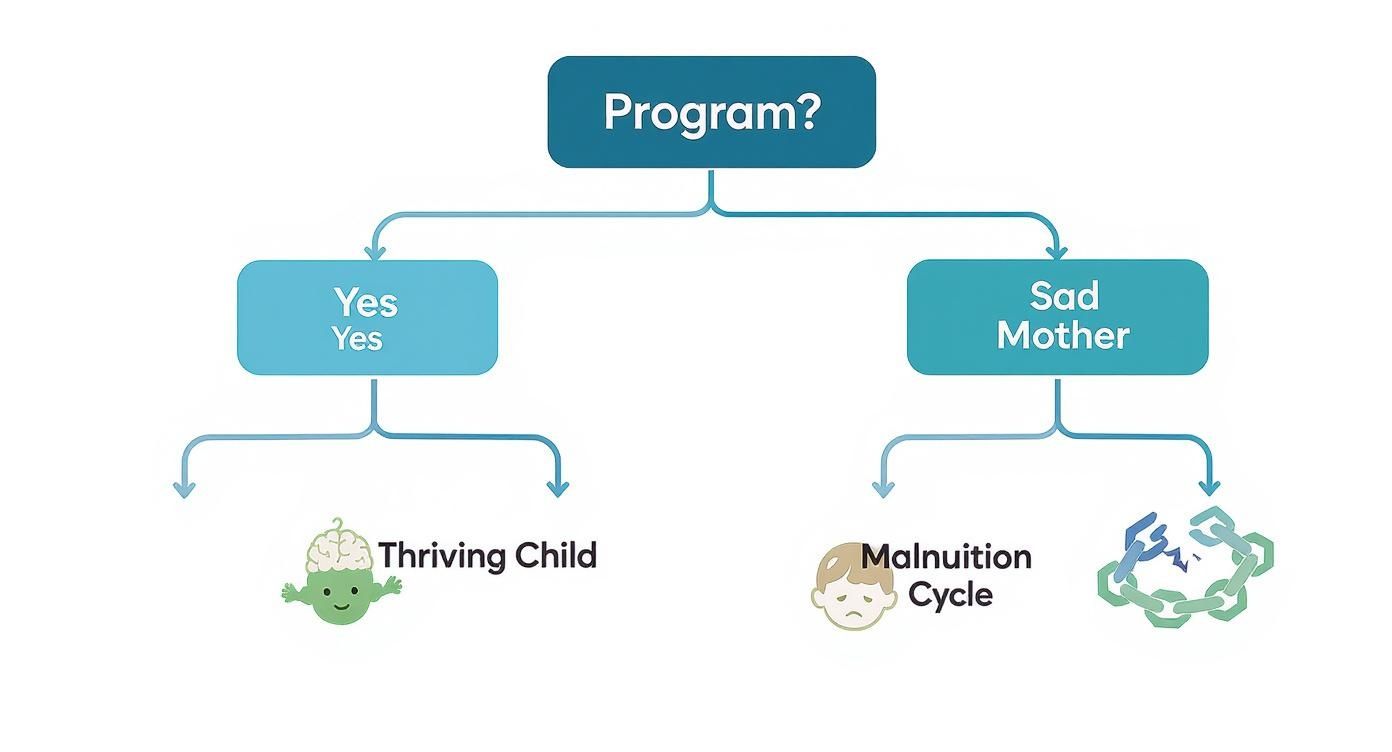
This fork in the road is a critical turning point. The presence of your program directly shapes the long-term health outcomes for the next generation.
Mastering Program Design and Delivery
The first big question is how you'll actually get food to families. There are a few proven models, and each comes with its own set of pros and cons.
- Medically tailored meals offer precise nutritional support for high-risk pregnancies, which is incredible. But they also demand serious culinary and logistical muscle.
- Food boxes or kits are a more common route. They provide shelf-stable groceries that families can cook with themselves, offering more flexibility and making it easier to scale up.
- Voucher systems empower participants with choice, letting them buy approved items at local stores. This approach requires strong partnerships with retailers and solid fraud prevention measures.
How do you pick? It really comes down to a few key factors like participant density, specific dietary needs (health conditions, cultural preferences), and the infrastructure you have access to.
Choosing the Right Nutrition Program Model
This table breaks down the primary models for delivering nutritional support, helping your organization select the best approach for your community's specific needs and resources.
| Program Model | Key Features | Best Suited For | Logistical Challenges |
|---|---|---|---|
| Medically Tailored Meals | Prepared, ready-to-eat meals designed by dietitians for specific health conditions (e.g., gestational diabetes). | High-risk participants needing strict dietary management; urban areas with dense delivery routes. | Requires commercial kitchen space, complex menu planning, refrigerated delivery fleet, and higher cost per person. |
| Food Boxes/Kits | Pre-packaged boxes of shelf-stable groceries, often with fresh produce add-ons. | Diverse populations with basic cooking facilities; programs needing to scale quickly across urban and rural areas. | Sourcing varied and culturally appropriate items, warehouse space for kitting, and managing volunteer or staff packing lines. |
| Voucher System | Electronic or paper vouchers redeemable for specific food items at partner grocery stores. | Communities with strong, accessible retail infrastructure; programs aiming to maximize participant choice and dignity. | Negotiating retailer agreements, managing fraud, tracking redemption data, and ensuring item eligibility is clear. |
Ultimately, the best model is the one that removes the most barriers for the mothers you serve, fitting realistically within your operational and financial constraints.
Securing Funding and Forging Partnerships
A brilliant program on paper doesn't mean much without the resources to make it happen. Funding is often the biggest hurdle. A great place to start is identifying grants from foundations, government agencies, and corporate sponsors that focus on public health and maternal wellness.
When you're writing those proposals, tell a compelling story backed by data. Clearly define the problem in your community, explain your solution, and detail exactly how you’ll measure success. Don't just lean on statistics; include anonymized anecdotes that bring the human impact of your work to life.
But money isn't everything—partnerships are just as vital.
- Medicaid and MCOs: Work with managed care organizations to frame your program as a preventative health benefit. Show them how it can lower medical costs tied to poor maternal nutrition.
- Local Food Banks: Don't view them as competition. Collaborate. Food banks can be incredible partners for sourcing food, sharing warehouse space, and coordinating distribution.
- Corporate Sponsors: Local businesses and grocery chains are often searching for meaningful ways to engage with the community. Pitch your program as a direct investment in the local workforce and future generations.
Navigating Logistics and Last-Mile Delivery
Once you have a model and funding, the real work starts. Managing the supply chain for a maternal nutrition program is all about careful planning. You’ll need to source high-quality, nutrient-dense foods, manage inventory to prevent spoilage, and build an efficient system for packing and distribution.
That "last mile" is almost always the toughest part of the puzzle. Reaching every single participant, especially those in remote or underserved areas, demands a rock-solid delivery strategy. This could mean your own fleet of vehicles, partnerships with third-party logistics (3PL) providers, or setting up convenient community pick-up points.
The ultimate goal is to remove barriers. Whether it's a lack of transportation, time, or childcare, the logistics of your program should make it easier—not harder—for a mother to get the food she needs.
Thinking through these operational details from day one is what elevates a well-intentioned idea into a sustainable, high-impact program. Every single step, from menu planning to delivery confirmation, helps build a system that mothers can truly depend on.
Coordinating with WIC and Overcoming Barriers
When you're running a maternal nutrition program, you don't have to reinvent the wheel. The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is a powerful, established system—it's a potential partner, not a competitor. Smart coordination can amplify your reach, prevent families from getting tangled in duplicate services, and create a truly seamless support network for mothers, especially those facing language and cultural barriers.
WIC is a massive pillar of public health. As the single largest buyer of infant formula in the country, it serves roughly 40% of all babies born in the United States. That's a huge footprint. The program already has the infrastructure, the participant relationships, and the nutritional guidelines. Your organization can build on that solid foundation, filling the critical gaps that federal programs can't always reach.
Building Seamless Referral Pathways with WIC
Real coordination starts with clear communication and a simple referral process. The goal should be a "no wrong door" approach, where a mother gets the help she needs no matter where she first shows up.
The first step is practical: meet with your local WIC agency directors. Go in ready to listen. What are their biggest headaches? Do moms have a hard time getting to their appointments because of transportation? Are they struggling with participant retention? Your program can be the solution to these very specific problems.
For example, your organization could offer to:
- Solve transportation hurdles: Provide ride-shares or bus passes so mothers can get to their WIC appointments without stress.
- Co-locate your services: Set up a desk at a WIC clinic one day a week to make enrollment into your food box or meal delivery program incredibly easy.
- Create a "warm handoff": Design a simple, shared referral form (with consent, of course). A WIC nutritionist can then directly connect a high-risk mother to your program for specialized support, like medically tailored meals for gestational diabetes.
Overcoming Language and Cultural Barriers
WIC agencies serve an incredibly diverse group of families but often lack the resources for deeply personalized, culturally specific support. This is where community-based programs can truly shine.
Focus on building trust by hiring staff who reflect the community. If your community has a large Spanish-speaking population, for example, it’s not enough to just translate a brochure. Hire bilingual staff who understand the cultural nuances around food, family, and health.
Your program can become the trusted bridge between a federal program and the community. By offering materials in multiple languages and designing food boxes with familiar cultural foods, you make nutritional guidance feel less like a prescription and more like a conversation with a knowledgeable neighbor.
This approach ensures vital information isn't just translated, but truly understood and embraced. For more on tailoring services to specific community needs, see how Umoja Health works with WIC programs. By filling these gaps, you enhance WIC's effectiveness and provide more holistic support. This also strengthens the support offered by WIC lactation consultants, especially when paired with resources like a guide on how to increase milk supply. To see how specialized food boxes can complement federal benefits, check out these kitting programs designed for seamless integration.
Creating a Program That Feels Like Home
A box of food can be a lifeline, but trust is what turns a service into a true support system. Effective maternal nutrition programs go beyond simply distributing calories; they build a sense of belonging and respect. To get there, programs have to move past checkbox solutions like basic translation and embrace genuine cultural connection. It's about making sure every mother feels seen, heard, and valued.

This means designing programs that don't just hand out food but offer nourishment in a way that feels familiar and comforting. The goal is to create something that feels less like an institution and more like a trusted extension of a mother's own community.
Navigating Language and Cultural Nuances
Overcoming communication barriers takes more than just Google Translate. True language justice is about ensuring genuine understanding, not just word-for-word translation. This often starts with hiring program staff who are native speakers and, ideally, members of the communities you serve.
These staff members become invaluable cultural liaisons, bridging gaps that a simple pamphlet never could. They understand the specific dietary staples, traditional postpartum recovery foods, and communication styles that build immediate rapport.
To really address cultural barriers, try these strategies:
- Community-Led Menu Design: Form a small advisory council of mothers from different backgrounds to help design and review menus. The most powerful question you can ask is, "What would you cook for your own family?"
- Visual Educational Materials: Develop recipe cards and nutritional guides that rely heavily on images and simple icons. This reduces the reliance on dense text and makes the information more accessible to everyone.
- Diverse Staffing: Prioritize hiring case managers, nutritionists, and delivery drivers who reflect the diversity of the families you partner with.
The most successful maternal nutrition programs operate on a simple principle: dignity. When a mother receives a box filled with ingredients she recognizes and knows how to cook, she feels respected. This simple act transforms the food from a handout into a thoughtful gift.
A Participant's Story: How Coordinated Support Changed Everything
Maria, a recent immigrant expecting her first child, felt completely isolated. She was enrolled in WIC but struggled to use the benefits—the approved foods were unfamiliar, and the language barrier during appointments left her feeling confused and deeply anxious about her baby's health.
Her WIC case manager referred her to a local maternal nutrition program that had a partnership with the agency. The difference was immediate. The program’s intake coordinator spoke her dialect and, more importantly, listened to her concerns with real empathy.
Soon, Maria started receiving weekly food boxes. Inside, alongside WIC-approved items like beans and rice, she found fresh cilantro, plantains, and masa harina—ingredients that reminded her of home. The box also included a simple, picture-based recipe for a nutrient-dense soup her own grandmother used to make for new mothers. For the first time in months, Maria felt a sense of relief and empowerment. The program didn't just provide food; it provided comfort, connection, and the confidence to nourish herself and her growing baby. Her story shows how a culturally thoughtful approach, working in harmony with established systems like WIC, can transform a participant’s experience from one of stress to one of strength.
How a Nutrition Program Changed Maria's Story

To really see how these programs work on the ground, let’s talk about a composite story based on the real experiences of participants. We’ll call her Maria. Her journey shows what’s possible when thoughtful, coordinated support turns a time of high anxiety into one of empowerment and health for both mother and child.
Maria was pregnant for the first time, in a city where she knew almost no one. The healthcare system felt overwhelming, and a constant worry gnawed at her: how could she provide enough good food for her growing baby? The stress was real. She’d often find herself skipping meals so her partner could eat a full dinner after a long day at work.
Finding a Lifeline Through Partnership
During a routine check-up, a sharp-eyed nurse noticed Maria’s stress and connected her with a local maternal nutrition program—one that worked hand-in-hand with her WIC office. That collaboration was everything. Instead of trying to figure out two different, confusing systems, Maria suddenly had a single, supportive network.
The program’s bilingual case manager sat down with her, patiently walking her through how the services worked together with her WIC benefits. The relief was instant. Maria wasn’t just given a box of food; she was welcomed into a community that truly saw her and understood her struggles.
"I thought I was completely alone in this. The first time they delivered a food box, I cried. It wasn’t just the food; it was knowing someone cared enough to help, to ask what I needed, and to speak to me in my own language."
More Than Just a Meal
This wasn’t just about groceries. The program’s entire approach was built on dignity and cultural respect, directly addressing the barriers that had made her feel so cut off.
- Culturally Connected Foods: Her weekly boxes weren’t random. They were filled with familiar ingredients like masa, beans, and fresh cilantro, which meant she could use her WIC benefits to cook the nourishing meals she grew up with.
- One-on-One Support: Her case manager became her go-to person, helping her schedule appointments, arranging transportation vouchers, and even connecting her with a peer group of other expectant moms.
- Bridging the Gap: The program staff acted as a bridge to WIC. They helped her understand which items were covered and shared recipes that used ingredients from both the program's food box and her WIC-approved list.
This coordinated effort was a game-changer. The constant worry about food just melted away, replaced by a sense of security. Maria’s health improved, and she felt more confident and ready for her baby’s arrival. Her story isn't just about food access. It's powerful proof of how integrated maternal nutrition programs can lighten a family’s stress, build real community, and lay the foundation for a healthy start in life.
How to Measure What Truly Matters
Gut feelings don't secure grant funding, but good data does. If you want to prove your maternal nutrition program is worth the investment, you have to move past the heartwarming stories and get serious about tracking outcomes.
This isn't just about checking boxes. It's about showing funders, healthcare partners, and your own team that the food you provide is making a clear, measurable difference in the health of moms and babies. A solid measurement plan is your best argument for keeping the program going and growing.
Key Metrics That Tell the Story
Your program does more than fill a pantry; it directly impacts health. The most powerful way to show your value is by tracking the changes in a few high-impact areas.
Focus your energy on collecting data that paints a clear picture of success from pregnancy through the postpartum period.
- Reduction in Low Birth Weight: This is a big one. Track the percentage of babies born to participants who are under 2,500 grams (5.5 pounds). Seeing this number go down is a huge win and a direct sign of better prenatal nutrition.
- Lower Anemia Rates: Anemia is incredibly common and draining for new moms. Measure hemoglobin levels when a mother joins your program and check in again after delivery. A drop in iron-deficiency anemia is a direct, tangible health improvement you can claim.
- Increased Breastfeeding Duration: Use simple surveys to ask moms how long they are breastfeeding, even if it's not exclusively. Longer durations mean your program is supporting both maternal health and infant nutrition long after the birth.
The trick is to gather meaningful data without overwhelming your staff or the families you serve. You don't need a massive research department. Simple surveys, partnering with clinics for optional health screenings, and even informal chats can give you incredibly rich information.
Put Your Numbers in a Global Context
Showing your local success is great, but framing it within a global health movement? That’s next-level. It makes your work feel bigger and more significant to funders who want to be part of a larger solution.
The World Health Organization (WHO) has set some major global nutrition targets for 2030. Two of the most relevant are a 50% reduction in anemia for women of reproductive age and a 30% reduction in low birth weight.
When you track your program's progress against these international goals, you change the entire conversation. You're no longer just running a local food service; you're on the front lines, helping solve one of the world's most critical public health challenges, one family at a time.
Your Top Questions on Program Implementation Answered
Getting a maternal nutrition program off the ground and running it effectively brings its own unique set of challenges. This final section tackles some of the most common questions we hear, offering clear, real-world advice to help you build a program that truly makes a difference.
Where Do I Even Begin Planning a New Program?
The first step isn't menus or funding—it's a deep dive into your community with a community needs assessment. You have to understand the specific hurdles, cultural foodways, and existing resources in your area before you do anything else. This foundational research will shape every single decision you make, from your delivery model to the partners you bring on board.
Get out and talk to people. Speak directly with local clinics, community leaders, and, most importantly, the families you hope to serve. This initial outreach is what separates a program that is truly wanted and needed from one that just looks good on paper.
How Can a Small Nonprofit Partner with WIC?
The key is to fill a specific gap that WIC doesn't—or can't—address. Don't try to duplicate their services. Instead, think about what you can offer that makes their jobs easier and improves the experience for the families they serve.
For instance, your program could step in to provide:
- Transportation to WIC appointments, which is a huge barrier for many families.
- Cooking classes that show moms how to use WIC-approved foods in recipes they already know and love.
- Specialized food boxes for high-risk mothers who have been referred directly by WIC nutritionists.
When you approach WIC, come with a clear value proposition. Show them exactly how you can help solve one of their persistent problems. That's how you build a strong, collaborative relationship that lasts.
What Wraparound Services Are Most Essential?
While food is the heart of any maternal nutrition program, wraparound services are what create lasting change. These services tackle the educational, emotional, and practical challenges of pregnancy and postpartum life, empowering mothers far beyond the food they receive.
"I came for the food, but I stayed for the support group. Talking with other new moms who understood what I was going through was a lifeline. It made me feel less alone and more confident." – A Participant's Story
Focus on services like one-on-one nutrition counseling, peer support groups where mothers can connect and share their stories, and access to lactation consultants. This holistic approach builds a powerful support system that nourishes the whole person, not just their physical health.
At Umoja Health, we specialize in helping organizations build and scale compliant, culturally connected food programs that communities can trust. Learn how we can support your mission.

