Medicaid 1115 waiver nutrition services are, at their core, a formal way for states to use Medicaid dollars for food-based interventions that tackle health-related social needs. These programs, which you’ll often hear called "Food is Medicine" initiatives, provide tangible support like medically tailored meals or produce prescriptions to improve people's health and, ultimately, bring down healthcare costs for eligible members.
Step 1: Understand the Policy Landscape and Why It Matters

Before you design a single program, you must understand the policy shift that makes it all possible. It's become impossible to ignore how conditions like diabetes, hypertension, and heart disease are deeply tangled up with whether someone can get their hands on healthy food. This growing awareness is the engine behind the "Food as Medicine" movement, which reframes nutrition as a critical piece of medical care, not just a lifestyle choice.
Medicaid Section 1115 demonstration waivers give states the green light to experiment with new ways to deliver care that aren't usually covered. For a long time, federal policy blocked Medicaid funds from being used for "room and board," a category that included food. But that's changing. States are now successfully arguing that targeted nutrition services can prevent expensive hospitalizations and help people better manage chronic conditions.
The Policy Shift Toward Food as Medicine
The momentum is undeniable. A recent analysis found that 19 approved and pending Section 1115 waivers now explicitly include nutrition services. This isn't a minor tweak; it's a major evolution in state-level health policy.
What’s really telling is that 11 of these waivers were submitted or approved just since 2021. This surge was kicked into high gear by the lessons learned during the COVID-19 pandemic and the spotlight from the 2022 White House Conference on Hunger, Nutrition, and Health.
This shift is a huge opportunity for organizations to finally address health issues at their foundation. By treating nutrition as a medical intervention, states are opening up new funding streams and forging vital partnerships between healthcare payers and community-based organizations.
These waivers aren't just about handing out food. They're about redesigning the entire system of care to be more holistic. The real goal is to create a system where a doctor can prescribe healthy meals just as easily as they prescribe medication, getting straight to the root causes of poor health.
What’s Driving This Change?
A few key factors are creating the perfect environment for these innovative nutrition programs to flourish. Across the board, states and health plans are zeroing in on:
- Cutting Chronic Disease Costs: It just makes sense. Proactively managing something like diabetes with the right diet can dramatically lower medical bills down the road.
- Tackling Health-Related Social Needs (HRSN): Food insecurity is one of the biggest HRSNs impacting health. Waivers offer a structured, fundable way to finally do something about it.
- Boosting Health Equity: These interventions can be aimed squarely at underserved communities that bear the brunt of diet-related diseases. Our guide on achieving community nutrition security goes much deeper into these strategies.
When you look at the bigger picture, including efforts for addressing critical public health challenges like childhood obesity, you can see just how powerful comprehensive nutrition services within Medicaid can be.
Common Nutrition Services in 1115 Waivers
So, what do these services actually look like in practice? States are getting creative, but a few models have emerged as the most common and effective. This table breaks down the most popular nutrition interventions you'll see in waiver applications, giving you a clear picture of what's gaining traction.
| Service Type | Description | Target Population Example |
|---|---|---|
| Medically Tailored Meals | Home-delivered meals designed by a dietitian to meet the specific nutritional needs of someone with a chronic illness. | An individual recently discharged from the hospital for congestive heart failure who needs low-sodium meals. |
| Produce Prescriptions | A prescription from a healthcare provider for fresh fruits and vegetables, redeemable at grocery stores or farmers' markets. | A pregnant person with gestational diabetes or a child identified as at-risk for obesity. |
| Food Pharmacies | On-site pantries, typically in a clinic or hospital, where patients can get healthy, often prescription-based, food for free. | A family experiencing food insecurity whose child has Type 1 diabetes and requires a consistent, healthy diet. |
| Medically Tailored Groceries | Providing a box of groceries selected to align with a person's health needs and dietary restrictions. | An adult managing kidney disease who needs foods low in potassium, phosphorus, and sodium. |
These service models represent the front lines of the "Food as Medicine" movement within Medicaid. They are practical, evidence-based approaches that connect the dots between nutrition and health outcomes, offering a tangible return on investment for states and a lifeline for members.
Step 2: Define Your Program Services and Target Populations

This is where your strategy takes shape. Designing your Medicaid 1115 waiver nutrition services program means defining exactly what you'll offer and who you'll offer it to. A well-designed program isn't just impactful—it must be administratively sound and compelling enough to get the green light from the Centers for Medicare & Medicaid Services (CMS).
The most successful programs start with a needs assessment. Dive into local health data to identify populations struggling with high rates of diet-related chronic conditions like diabetes or heart failure. This data-driven approach is non-negotiable.
Choosing the Right Service Models
After you've identified your target groups, you can start matching them with the right nutrition interventions. There's no single "best" model here; what works depends entirely on the specific needs of the people you're trying to help. Most states tend to focus their efforts on a few proven approaches.
- Medically Tailored Meals (MTMs): These are the heavy hitters—fully prepared, home-delivered meals designed by a Registered Dietitian to manage a specific medical condition. They're a perfect fit for folks just discharged from the hospital or those who have a tough time cooking for themselves.
- Healthy Grocery or Produce Boxes: This model is fantastic for families or individuals who know their way around a kitchen but face real barriers to accessing or affording healthy food. It's a box of curated healthy groceries or fresh produce delivered right to their door.
- Produce Prescriptions (PRx): Here, a healthcare provider actually "prescribes" fresh produce. Members can then use vouchers or cards to get that produce from participating grocery stores or farmers' markets. This approach really empowers member choice and has the added benefit of supporting local food systems.
- Nutrition Education and Counseling: This is often the glue that holds other services together. It's about giving members the knowledge and skills to make healthy choices that stick. When thinking about the full spectrum of services, programs might offer resources on different dietary approaches, like providing specific dietary meal plans designed for various health needs.
Pinpointing Your Target Population with Precision
Defining your target population and eligibility criteria is probably the most critical part of your waiver proposal. If you're vague, you're setting yourself up for implementation nightmares and lackluster outcomes. The goal is to create clear, data-driven criteria that draw a straight line between the nutrition service and a specific health need.
From our experience, the programs that get results are laser-focused on high-priority groups where nutrition can move the needle in a measurable way.
Key Insight: Don't just target "food insecurity." Instead, target a clinical population experiencing food insecurity. For example, specify "Medicaid members with uncontrolled Type 2 diabetes (HbA1c > 8.0) who also screen positive for food insecurity." This ties the social need directly to a Medicaid-relevant health metric.
For instance, a state might zero in on pregnant individuals to improve birth outcomes, or on members with behavioral health conditions, where stable nutrition can be a game-changer for treatment adherence. Specificity is your friend.
We're seeing states get more and more targeted. Look at Pennsylvania's proposed Section 1115 waiver—it introduces services like grocery delivery specifically for pregnant and postpartum Medicaid enrollees. This isn't coming out of left field; it builds on established, CMS-approved strategies and echoes what New York has done successfully with its waiver for high-risk pregnant individuals.
This level of detail is what shows CMS you've built a thoughtful health intervention, not just another general food program. It also makes it worlds easier to measure your impact, which is absolutely essential if you want your program to be sustainable in the long run. And for organizations working with younger populations, understanding the nuances of various initiatives is key. You might find our guide on implementing effective child nutrition programs helpful.
Step 3: Craft a Winning Waiver Application
Think of your Medicaid 1115 waiver application as more than just paperwork. It’s your strategic pitch—your story. The goal is to build a rock-solid case showing how your proposed Medicaid 1115 waiver nutrition services will hit key Medicaid objectives, like improving health outcomes while being smart about costs.
Frankly, you're building a business case for investing in food as medicine.
Applications that get the green light always stand on three pillars: a powerful evidence base, clear and compliant language, and a budget-neutral financial model. CMS needs to be confident you've done the legwork and that your plan is both effective and fiscally sound. This isn't just about asking for money. It's about presenting a targeted health intervention that uses nutrition to tackle expensive problems.
Build Your Evidence Base First
Before you even start writing, you have to gather your proof. CMS wants to see that your program is built on a foundation of solid evidence, not just good intentions. This is where you draw a straight line from the services you want to provide to the results you expect to see.
Your evidence should come from a few key places:
- Relevant Studies: Dig into the established research that connects your chosen interventions—like medically tailored meals or produce prescriptions—to better health outcomes for your specific population. For instance, you could cite studies showing how MTMs led to reduced HbA1c levels in people with diabetes.
- Pilot Program Data: If you've run a smaller pilot, that data is pure gold. Showcase your own results, even if they’re preliminary. Things like better member engagement, fewer ER visits, or positive biometric changes are incredibly persuasive.
- State-Specific Health Data: Use local data to paint a vivid picture of the problem you’re solving. Highlighting high rates of diet-related diseases in certain counties or demographic groups makes your targeted approach feel necessary and urgent.
A common mistake is making a generic argument for nutrition. You have to be specific. Instead of saying, "Healthy food improves health," your application needs to say something like, "Providing 12 weeks of medically tailored groceries to post-discharge congestive heart failure patients is projected to reduce hospital readmission rates by 15%, based on findings from a similar pilot in North Carolina."
Get the Language Right
The words you use in your waiver application must be precise and carefully aligned with federal Medicaid guidelines. Every sentence should drive home the point that your nutrition program is a legitimate healthcare service.
Here’s some sample language for a service definition:
"The proposed Medically Tailored Grocery service is a nutritional intervention designed to manage and treat diet-related chronic conditions among eligible members. This service provides a weekly box of groceries, selected by a Registered Dietitian, that directly supports the member's prescribed dietary plan for conditions such as Type 2 diabetes and hypertension."
And for an eligibility pathway:
"Eligibility for nutrition services is limited to Medicaid members with a qualifying clinical diagnosis (e.g., congestive heart failure, uncontrolled diabetes) who also screen positive for food insecurity via a validated screening tool. A referral from a treating clinician is required to initiate services, ensuring the intervention is integrated into the member's comprehensive plan of care."
This kind of language frames the service exactly how CMS needs to see it: as a targeted, clinically appropriate treatment worthy of Medicaid funds.
Prove It Won't Cost More
Finally, your application must demonstrate that the waiver won't cost the federal government more than it would have spent otherwise. This is the budget neutrality requirement, and it's an absolute deal-breaker.
Your financial model needs to project how the costs of your nutrition services will be offset by savings in other areas. Typically, these savings come from:
- Fewer hospital admissions and readmissions.
- A drop in emergency department visits.
- Less need for intensive and expensive medical procedures.
This is where you need to work closely with actuaries and health economists to build a credible financial forecast. Forging a strong partnership between Managed Care Organizations (MCOs) and Community-Based Organizations (CBOs) is absolutely critical here. MCOs have the claims data to model potential savings, and CBOs have the on-the-ground expertise to deliver the services. That collaboration is the key to creating a financially sound proposal that has the best shot at getting approved.
Step 4: Develop Your Implementation Blueprint for Launch
Getting the green light for your Medicaid 1115 waiver nutrition services program is a massive win, but as anyone who's been there knows, the real work is just beginning. This is the moment your carefully crafted proposal needs to become a living, breathing operation that gets real food to real people. A well-thought-out implementation plan is what separates a program that thrives from one that gets tangled in logistical knots.
Making that leap from paper to practice demands a sharp, operational roadmap. You'll be navigating everything from vendor procurement and contract negotiations to the nitty-gritty details of referral workflows. The aim is to build a system that's not only compliant but also feels completely seamless for the members you're serving.
Building Your Partner and Vendor Ecosystem
Let's be clear: you can't do this work alone. Your program's success is riding on a strong network of partners—food vendors, community-based organizations (CBOs), and maybe even technology providers. Choosing these partners is one of the most critical calls you'll make.
When you're vetting potential food vendors, you have to look beyond a simple price sheet. Dig into their capacity to scale, their track record with special dietary needs, and their fluency in compliance. For instance, if medically tailored meals are part of your plan, your vendor absolutely must have Registered Dietitians on staff who can oversee menu creation and ensure every meal hits strict clinical targets.
As for CBOs, you want organizations with deep roots and trusted relationships in the communities you're trying to reach. They are your boots-on-the-ground, your outreach and engagement arm. They're essential for everything from enrolling members to handling that crucial last-mile delivery.
Expert Tip: Never, ever underestimate the complexity of food logistics. When you're talking to vendors, ask specific, pointed questions about their cold-chain management. A single breakdown in keeping perishable items at the right temperature can jeopardize food safety and instantly shatter the trust you've built with your members.
Crafting Ironclad Contracts and Workflows
Once your dream team of partners is in place, it's time to get everything in writing with clear, effective contracts and service level agreements (SLAs). Vague agreements are a recipe for disaster, leading to confusion and subpar performance. Your contracts need to spell out every detail with precision.
Your SLAs, in particular, must clearly define:
- Key Performance Indicators (KPIs): Be specific. This means metrics like on-time delivery rates (e.g., 98% of meals delivered within the agreed-upon window) and order accuracy.
- Data Sharing Protocols: Lay out exactly what data needs to be shared, how often, and in what format. This is non-negotiable for your reporting back to the state and CMS.
- Referral Workflow: Map out the entire journey, from the second a healthcare provider makes a referral to the moment the first food delivery is made. Who owns each step? What's the maximum turnaround time allowed?
The process flow below gives you a high-level view, from defining your program's purpose to proposing a concrete solution.
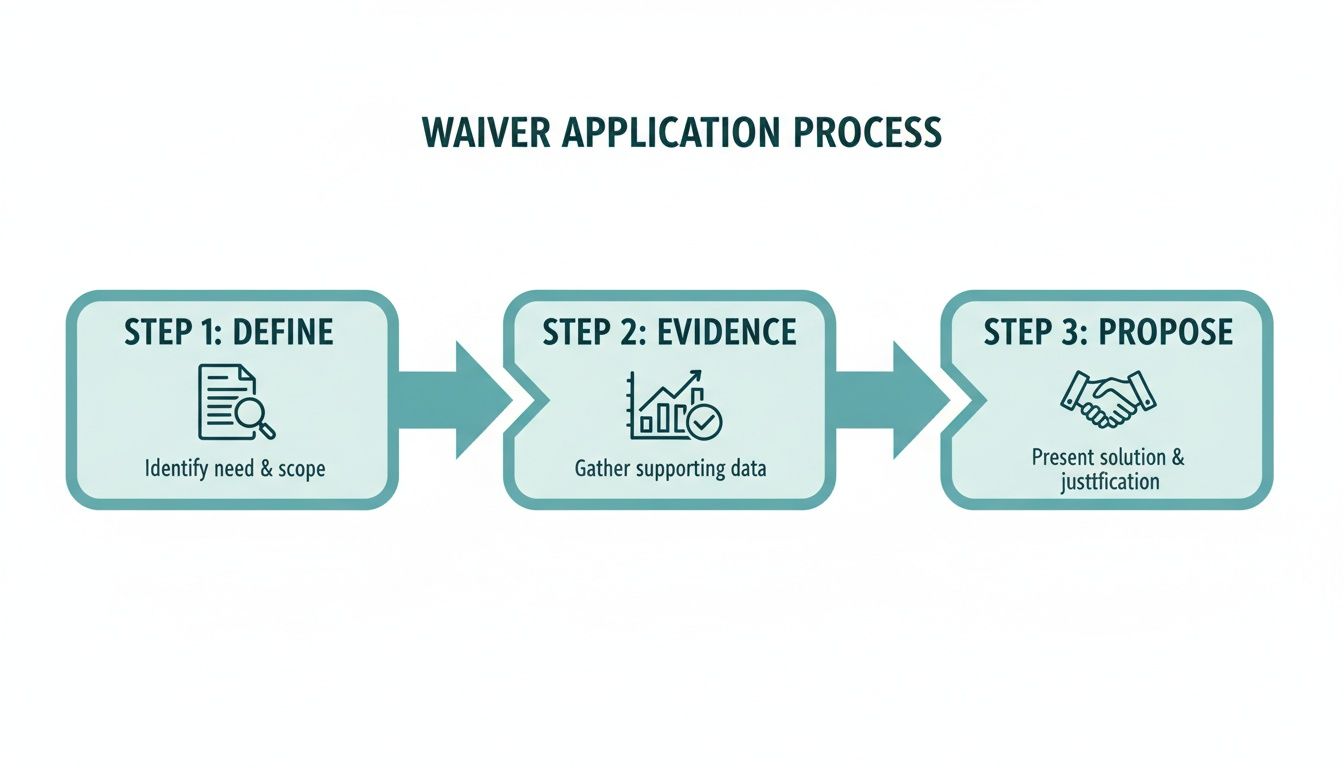
This kind of structured approach ensures that every phase, from initial concept to final proposal, is built on a solid foundation of clear goals and compelling evidence.
Mastering the Logistics of Food Delivery
The final piece of the implementation puzzle is the physical act of getting food to doorsteps. This is where many well-intentioned programs hit unexpected roadblocks. You have to think about everything—warehousing, inventory management, route optimization, and even proof of delivery.
For shelf-stable items, things are a bit more straightforward. For those looking to manage this process efficiently, diving into the mechanics of food kitting programs can offer a great framework for assembling and distributing packages at scale.
But for perishable goods like fresh produce or frozen meals, cold-chain management is the name of the game. It's not optional. This means maintaining a consistent, safe temperature from the warehouse, onto the truck, and all the way to a member's front door. That requires specialized gear like refrigerated vans and insulated packaging, adding layers of complexity and cost that you must bake into your operational model from day one.
Your Nutrition Program Implementation Checklist
To help you stay on track, we've put together a practical checklist that walks you through the key operational phases of getting your 1115 waiver nutrition program off the ground. Think of this as your guide from planning to launch.
| Phase | Key Action Item | Considerations and Best Practices |
|---|---|---|
| 1. Procurement & Contracting | Identify and vet food vendors, CBOs, and tech partners. | Look for experience with Medicaid populations. Ask for references. Scrutinize their capacity for scale and compliance (e.g., HIPAA). |
| Draft and execute detailed contracts and SLAs. | Define specific KPIs (delivery times, order accuracy), data sharing protocols, and clear payment terms. Involve legal counsel. | |
| 2. Workflow & Systems | Design the end-to-end referral and enrollment process. | Map every touchpoint. Define roles and responsibilities for MCOs, providers, CBOs, and vendors to ensure no one falls through the cracks. |
| Set up data systems for tracking, reporting, and billing. | Ensure systems can capture all required metrics for CMS reporting. Test data integrations between partners before launch day. | |
| 3. Logistics & Operations | Establish food sourcing, warehousing, and inventory plans. | Address "Buy American" provisions if applicable. Plan for supply chain disruptions. Secure adequate storage space. |
| Finalize the "last-mile" delivery model. | Confirm cold-chain protocols for perishables. Develop a communication plan for members regarding delivery windows and potential delays. | |
| 4. Training & Launch | Train all staff and partners on workflows and protocols. | Conduct joint training sessions to ensure everyone understands their role and how it connects to others. Provide clear documentation. |
| Run a small-scale pilot program before full launch. | Test every aspect of your operation with a small group of members to identify and fix issues before scaling up. |
Planning for these logistical realities isn't just good practice—it's absolutely essential for a successful and sustainable launch that truly makes a difference.
Step 5: Measure Impact and Prove Your Program's Value

If you want your Medicaid 1115 waiver nutrition services to stick around, you have to prove they work. A powerful measurement and evaluation framework isn’t just a box to check for reporting. It’s the lifeblood of your program’s sustainability. This means you have to move beyond feel-good stories and build a rock-solid case with data.
Your mission is to show a clear return on investment (ROI) to your state Medicaid agency and CMS. They need to see that putting money into medically tailored meals or produce prescriptions directly translates to better health outcomes and, just as importantly, lower overall healthcare spending.
Defining Key Performance Indicators That Matter
The first move is picking the right Key Performance Indicators (KPIs). Your focus should be on a balanced set of metrics that tell a complete, compelling story, from how members are engaging to the actual clinical and financial impact.
A strong M&E plan usually zeroes in on metrics across three core areas:
- Process Metrics: These are your day-to-day operational health checks. Think referral acceptance rates, member enrollment and retention, and on-time delivery percentages. They show your program is running smoothly.
- Health Outcome Metrics: This is where you connect your services to clinical changes. You're showing your program is actually making people healthier. We're talking about improvements in HbA1c levels for members with diabetes, drops in blood pressure, and changes in BMI or weight.
- Healthcare Utilization Metrics: These are the heavy hitters for proving ROI. They demonstrate how your program is bending the healthcare cost curve. The most persuasive metrics here are a reduction in emergency department (ED) visits, fewer inpatient hospital admissions, and a decrease in 30-day hospital readmission rates.
Building a compelling case means connecting the dots. It’s about showing that high member engagement (a process metric) leads to better HbA1c control (a health outcome), which in turn results in fewer costly ED visits (a utilization metric). That’s the narrative that secures long-term funding.
Collecting and Analyzing Your Data
Once your KPIs are locked in, you need a solid data collection plan. This is rarely a single-source job; you'll need to pull information from various places. That means getting data-sharing agreements in place with your partners, including healthcare providers, MCOs, and the community-based organizations actually delivering the food.
Common ways to gather this data include:
- Claims Data Analysis: Your MCO partners can provide claims data to track healthcare utilization—like hospital stays and ED visits—before and after a member starts receiving nutrition services.
- Biometric Screenings: Work with clinics or use in-home services to capture hard clinical data like blood pressure, weight, and HbA1c levels at the beginning, middle, and end of the program.
- Member Surveys: Don't underestimate the power of self-reported data. Use validated screening tools and satisfaction surveys to measure changes in food security, perceived health, and their overall experience.
A Real-World Case Study in Proving Value
Seeing how other states have tackled this can be incredibly helpful. Take Massachusetts' Flexible Services Program, a "Food Is Medicine" initiative under its 1115 waiver. They provided nutritional support to over 20,000 participants.
What did they find? Post-2021 evaluations showed the program successfully cut down on both emergency department visits and inpatient stays. This was clear proof of a positive impact on member health and healthcare costs. Findings like these help validate Section 1115 waivers as cost-effective tools for social interventions. It’s worth exploring their full findings to see exactly how they measured and presented this impact.
By meticulously tracking the right metrics and telling a clear story with your data, you can transform your program from a promising pilot into an evidence-based, indispensable part of the healthcare system. This rigorous approach is what turns a temporary waiver project into a permanent, funded solution.
Your Top Questions on Nutrition Waivers, Answered
Once organizations start digging into Medicaid 1115 waiver nutrition services, the same practical questions pop up time and again. I've been in these conversations, and getting straight answers is the only way to move from a great idea to a successful, running program. Let's tackle the big ones head-on.
These questions usually get right to the heart of the matter—the money, the logistics, and the biggest operational headaches you're likely to face.
How Does the Money Actually Flow for These Services?
Let's clear this up right away: funding for nutrition services under an 1115 waiver isn't a grant. The money typically moves from the state Medicaid agency to Managed Care Organizations (MCOs) as part of their capitated rates. Those are the fixed, per-member, per-month payments MCOs get for covering a patient's care.
From there, the MCOs contract with and pay community-based organizations (CBOs) or other food partners to deliver the actual services, whether it's medically tailored meals or produce boxes. While you might see some direct fee-for-service models out there, this MCO-to-CBO partnership is quickly becoming the standard way to do things.
It's absolutely crucial to remember that the waiver has to prove budget neutrality. This means the cost of adding new nutrition services has to be balanced out by savings somewhere else—think a projected drop in expensive hospital stays or ER visits for the people you're serving.
How Long Can Someone Actually Get These Nutrition Benefits?
This isn't a one-size-fits-all answer. The duration of services depends on the state and is spelled out in the waiver's Special Terms and Conditions (STCs). For a long time, the unofficial CMS guidance pointed to a six-month limit, maybe with a six-month extension if you were lucky.
But that's changing. We're seeing states successfully propose—and get approval for—much longer service periods, as long as they're backed by a solid clinical need.
Take the waivers aimed at pregnant and postpartum individuals, for example. Waivers approved in New York and proposed in Pennsylvania are looking at services that can last up to 11 months. This covers the entire perinatal period, a critical window for health. The key is building a powerful case with clinical evidence that shows why that specific duration is necessary to get the health outcomes you’re aiming for.
Can We Really Use Waiver Funds to Pay for the Food Itself?
Yes, and honestly, this is one of the most important shifts we've seen in recent 1115 waivers. For years, federal funds were blocked from covering "room and board," which included food. But CMS has changed its thinking. Now, waivers are getting the green light to cover the cost of food when it's part of a direct medical intervention or therapeutic service.
Think of it this way: medically tailored meals aren't just a food supplement. They're framed as a specific treatment for a health condition, just like a prescription.
To get this approved, your waiver application has to meticulously define the nutrition service as a core part of a patient's care plan. It has to be positioned as a tool to treat a medical condition or hit a specific health goal, not just a general food benefit.
What Are the Biggest Hurdles in Getting These Programs Off the Ground?
Moving from an approved waiver on paper to a fully functioning program in the real world is where the real work begins. Based on my experience helping organizations on the ground, a few challenges come up over and over again.
- Getting the Data Right: Building a secure and reliable way for healthcare providers (who write the "prescriptions") to share data with CBOs (who deliver the food) is a massive technical and administrative lift.
- The Logistics Puzzle: Don't underestimate the complexity of managing food sourcing and delivery. Cold-chain management for fresh, perishable food requires real expertise and the right equipment. It's much more than just dropping off a box.
- Billing and Getting Paid: For many CBOs new to the healthcare world, navigating the labyrinth of MCO billing and reimbursement can feel like learning a new language. It’s a steep learning curve.
- Engaging the Community: Just because someone is eligible doesn't mean they'll sign up. It takes effective, culturally sensitive outreach and genuine trust-building to get people enrolled and keep them participating.
And finally, perhaps the biggest challenge of all is figuring out sustainable, long-term funding after the initial waiver period ends. This means you have to be obsessed with collecting data and proving a clear return on investment right from day one.
At Umoja Health, we live and breathe these complexities. Whether it's designing culturally connected, medically appropriate food boxes or providing the logistical backbone for large-scale distribution, we help organizations build and run compliant, impactful nutrition programs. Find out how we can help you at https://umojahealth.com.