You can’t just hand someone a pamphlet and expect their health to change. Effective nutrition education programs in healthcare are clinical interventions designed to improve patient outcomes, manage chronic diseases, and lower long-term medical costs. This planner provides a step-by-step guide for health organizations to design, launch, and sustain programs that make nutrition a true pillar of health.
Why Nutrition Education Is a Healthcare Essential

Moving beyond vague advice to “eat healthy” is a strategic imperative for any modern healthcare organization. The conditions driving the majority of healthcare spending—diabetes, hypertension, heart disease—are all directly tied to diet. Giving patients structured, practical education empowers them with the skills to manage their own health through food.
This proactive approach directly addresses the financial strain on our health systems. When patients learn how to control their blood sugar with smarter food choices or lower their blood pressure by cutting sodium, the results are tangible: fewer ER visits, lower hospital readmission rates, and less reliance on costly medications. It fundamentally transforms the care model.
The Food as Medicine Model
The “Food is Medicine” movement isn’t just a trend; it reframes nutrition as a core part of a patient’s treatment plan. It’s based on the premise that access to healthy, appropriate food is just as critical as any prescription. This is where well-designed nutrition education programs in healthcare deliver the greatest impact.
Here’s why it works:
- Improved Clinical Outcomes: We see measurable improvements in key biomarkers, like A1c levels, blood pressure readings, and cholesterol.
- Increased Patient Engagement: Providing hands-on, practical guidance builds a stronger, more trusting relationship between patients and providers. It gives people the confidence to take an active role in their own health journey.
- Lower Healthcare Costs: Preventative care through nutrition simply costs less. It dramatically reduces the need for expensive, intensive interventions down the road.
Before building your program, it’s helpful to understand the key pillars that make these initiatives successful and scalable.
| Component | Objective | Key Activities |
|---|---|---|
| Clinical Integration | Embed nutrition into the standard care workflow. | Include nutritionists on care teams; build EHR flags for at-risk patients; add nutrition goals to treatment plans. |
| Personalized Education | Provide guidance that is relevant to the individual. | Offer culturally-relevant meal plans; create condition-specific materials (e.g., for diabetes, renal disease); conduct one-on-one counseling. |
| Food Access | Remove barriers to obtaining healthy food. | Partner with medically tailored grocery providers; establish produce prescription programs; coordinate with community food banks. |
| Measurement & Outcomes | Track progress to prove value and refine the program. | Monitor clinical data (A1c, BP); collect patient-reported outcomes (PROs); track engagement and adherence rates. |
A program built on these four components doesn’t just inform patients; it actively supports their journey to better health.
A Growing Global Priority
This intense focus on nutrition isn’t happening in a vacuum. The U.S. Bureau of Labor Statistics expects employment for nutrition professionals to jump 7% by 2032. This mirrors a global push, with organizations like the World Health Organization (WHO) making nutrition education a core strategy to hit worldwide health targets for 2030, including reducing conditions like stunting and anaemia. You can see the full scope of these global nutrition targets here.
Umoja Tip: We’ve learned that the most successful programs are those deeply integrated into the clinical workflow. When a nutritionist or a Community Health Worker is part of the care team, education becomes a continuous dialogue rather than a one-time consultation. This consistent support is what drives lasting behavioral change.
Planning Your Curriculum: A CHW-Powered Approach

A world-class nutrition program will fall flat if the curriculum doesn’t connect with the real lives of your participants. The goal is to move past generic advice and create culturally competent, practical materials that patients will actually use. This means designing a curriculum that understands their environment, respects their background, and provides actionable skills.
Effective nutrition education programs in healthcare are built on empathy and practicality. This starts by recognizing that what ends up on the plate is shaped by more than simple choice—it’s about income, transportation, cultural traditions, and a dozen other daily realities.
Core Components for a CHW Curriculum
Community Health Workers (CHWs) are the most trusted messengers in these programs. A powerful curriculum should focus less on lecturing and more on fostering genuine connection and motivation.
At Umoja, we build our CHW training around these core components:
- Motivational Interviewing: Instead of telling patients what to do, CHWs learn to ask powerful questions. This collaborative approach helps patients find their own reasons for change, which makes new habits far more likely to stick.
- Hands-On, Practical Learning: Training must simulate the real world. This means role-playing patient conversations, practicing goal-setting exercises, and learning how to navigate tough discussions about social determinants of health.
- Cultural Humility Training: Equip CHWs to understand and respect diverse cultural foodways. The curriculum should teach them to adapt nutritional guidance to fit different cuisines and traditions, rather than imposing a one-size-fits-all diet.
When you equip CHWs with these skills, they become effective health coaches who can guide patients on a deeply personal journey.
From Aisle to Kitchen: Creating Shoppable Guides
One of the biggest hurdles for patients is turning a doctor’s advice into an actual grocery list. A standard food pyramid is useless if the recommended items aren’t available or affordable at their local store.
Umoja Tip: We create “shoppable” nutrition guides that literally mirror the layout of local grocery stores. By organizing recommendations by aisle—produce, canned goods, frozen foods—we cut down on the mental effort and make healthy shopping feel intuitive and achievable.
This hyper-local approach builds immediate trust and proves your program is designed for their success. These are the practical tools that turn knowledge into action.
Addressing Health Literacy and Social Needs
People absorb information in different ways. A curriculum that works must be tiered to accommodate different levels of health literacy and address social barriers to healthy eating.
Plan a range of resources:
- Visual Aids: For people with low health literacy, simple, picture-based guides on portion sizes or reading food labels can be a game-changer.
- Interactive Workshops: Group classes on budget-friendly meal prep or cooking for a specific condition (like diabetes) build skills and a sense of community.
- In-Depth Counseling: One-on-one sessions are critical for patients with complex medical needs or significant social barriers.
This tiered structure ensures your message connects with everyone. The global impact of these integrated strategies is huge. By 2025, targeted nutrition initiatives are projected to reach 100,000 employees worldwide, and in 2023, 70% of major nutrition programs were multi-sectoral, blending health with social support and education. This philosophy extends to resource delivery; see how kitting programs can enhance nutrition security to link tangible food access with your educational efforts.
Planning for Telehealth Adaptation
Moving a hands-on service like nutrition education online can feel like a huge leap. How do you keep that genuine human connection through a screen? Going virtual is about more than choosing a HIPAA-compliant video tool. It’s a chance to rethink engagement so your nutrition education programs in healthcare are just as effective and accessible as in-person services.
Shifting to telehealth can break down barriers like transportation and childcare. But it also creates the challenge of the digital divide. A successful virtual program must be built with equity in mind.
Strategies for Digital Engagement
Keeping patients motivated from a distance means thinking beyond the scheduled video call. Consistent, low-effort touchpoints are the secret sauce for reinforcing new habits between formal sessions.
Here are battle-tested ideas to incorporate into your plan:
- Text-Based Nudges: Simple, automated texts can be incredibly powerful. A morning message might offer a quick recipe idea. An afternoon nudge could be a gentle reminder to hit a walking goal.
- The Virtual Pantry Makeover: A fantastic, personal telehealth activity. A nutritionist or CHW can have a patient use their phone camera to give them a tour of their pantry and fridge for real-time advice on reading labels and making smarter swaps.
- Group Video Support: Weekly group video calls build powerful peer networks. When patients share wins, talk through challenges, and see they aren’t alone, it creates a massive boost in motivation.
For a solid framework to structure your digital curriculum, exploring a practical guide to online learning and virtual training can be invaluable for turning passive information into active learning.
Bridging the Digital Divide
Not every patient has high-speed internet or feels comfortable on a video call. An equitable telehealth strategy must meet this reality head-on with a spectrum of communication options.
Umoja Tip: We build our programs with a “no-tech to low-tech” philosophy. Every digital resource should have an analog counterpart. This simple rule ensures that a patient’s access to care is never dependent on their access to technology.
For example, a digital meal planner is great, but a printable, mail-out version is essential. A live cooking demo on Zoom is engaging, but a step-by-step recipe guide with clear photos sent by mail is just as powerful for someone offline.
Don’t forget these practical, low-tech alternatives:
- Phone-Based Coaching: Never underestimate the power of a simple phone call. For many patients, it remains the most accessible and personal way to connect.
- Mail-Out Materials: High-quality printed resources are non-negotiable. Think newsletters, recipe cards, and worksheets that directly support topics covered in virtual or phone sessions.
- Interactive Voice Response (IVR): For larger programs, automated IVR systems can deliver daily health tips or short educational messages that patients can listen to on their own time, no internet required.
By blending high-tech and low-tech approaches, you create a resilient program that adapts to the real-world needs of every person you serve. Find more insights on building adaptable healthcare solutions in our thought leadership articles.
Mastering Your Program Logistics: An Operational Playbook
A brilliant curriculum and dedicated team are essential, but the success of nutrition education programs in healthcare often comes down to logistics. Without a solid operational backbone, even the best plans can fall apart. This playbook covers seamless workflows, food distribution complexities, and ensuring a smooth patient experience. When logistics are right, they’re invisible to the patient.
Designing a Seamless Patient Workflow
A clunky enrollment process can kill momentum. The workflow must be baked directly into your existing clinical practice.
- Screening at Intake: Integrate simple food insecurity screening questions—like the Hunger Vital Sign™—into standard intake forms to automatically flag at-risk patients for your care team.
- Warm Handoffs: Once a patient is identified, don’t just hand them a flyer. A “warm handoff,” where a clinician personally introduces the patient to a CHW or program coordinator, dramatically boosts enrollment rates.
- Clear Onboarding: Create a simple onboarding packet covering the program schedule, contact info for their CHW, and what to expect in the first few weeks. This cuts down on confusion and sets realistic expectations.
Keeping track of everything requires good systems. Tools like medical documentation software can be incredibly helpful for streamlining patient records and cutting down on administrative headaches.
The Nuts and Bolts of a Food is Medicine Grocery Model
If your program provides direct access to food, the logistical puzzle gets more complex. Running a “Food is Medicine” grocery model means juggling sourcing, inventory, and distribution.
This infographic shows how you can adapt your education program for a telehealth world, keeping that virtual connection and reinforcement strong.
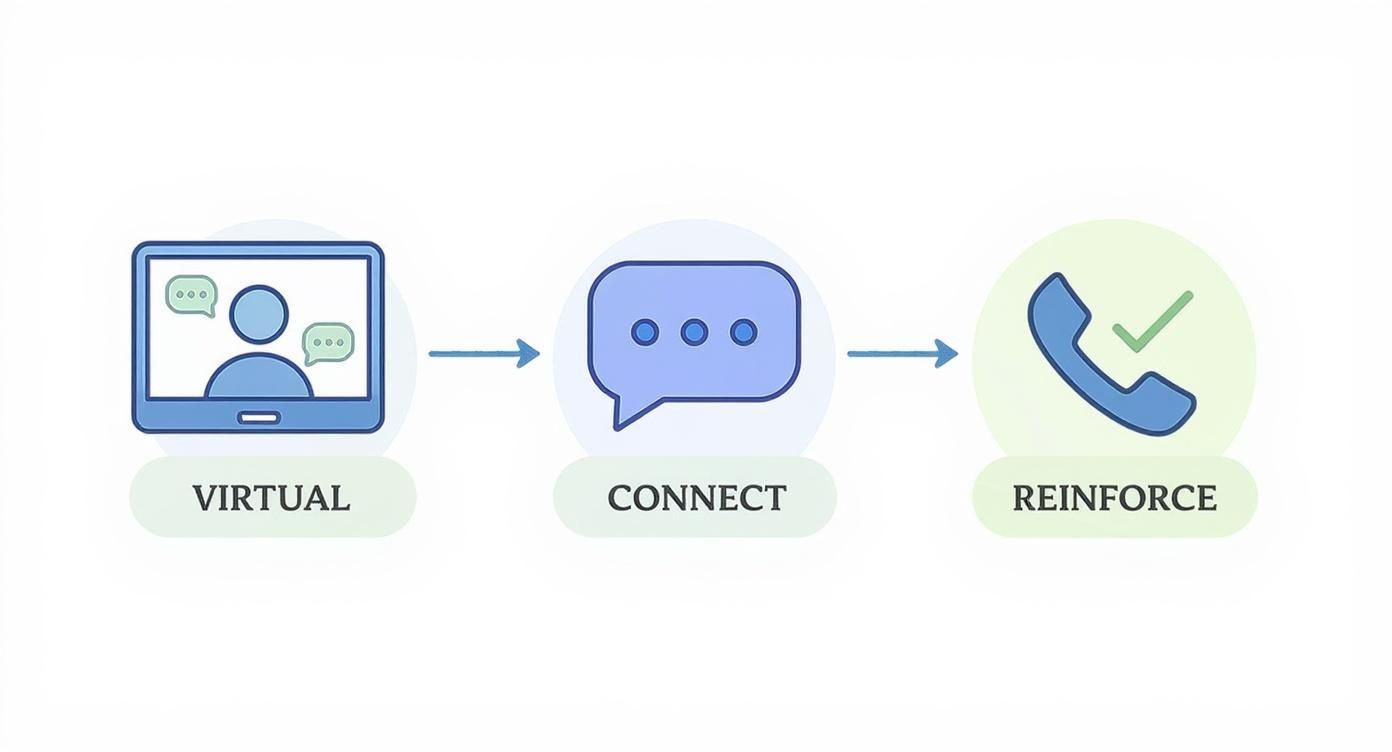
This visual flow illustrates how tech can maintain supportive, continuous contact with patients, even when they’re not physically in your clinic. A critical note: patient data is non-negotiable. Ensure every partner in your supply chain is HIPAA-compliant and has ironclad data security protocols.
Choosing Your Distribution Model: Pick-Up vs. Delivery
How you get food to your patients is a pivotal decision. The right choice depends on your patient population, geography, and resources.
A pick-up model can build community and allow for face-to-face time with staff. The downside is the transportation burden on the patient, which can be a significant barrier.
A delivery model offers maximum convenience and removes that transportation barrier, but it comes with higher costs and logistical hurdles like route planning and ensuring food safety in transit.
Delivery vs Pick-Up Model Comparison
Use this table to weigh the pros and cons for your specific program.
| Factor | Delivery Model | Pick-Up Model |
|---|---|---|
| Accessibility | High; removes transportation barriers for patients. | Lower; requires patients to travel to a central location. |
| Cost | Higher; includes fuel, driver time, and vehicle maintenance. | Lower; fewer direct costs, relies on existing site infrastructure. |
| Patient Engagement | Lower potential for face-to-face interaction. | Higher; creates opportunities for in-person support and community. |
| Logistics | Complex; requires route optimization and managing no-shows. | Simpler; centralized distribution with predictable schedules. |
Often, a hybrid approach works best. Offer a central pick-up location but reserve delivery for your most vulnerable or geographically isolated patients. This can be a cost-effective and equitable solution.
No-shows are a common headache. We’ve seen that implementing a simple text-based reminder system 24 hours before a scheduled delivery or pick-up can cut missed appointments by over 30%, saving time and resources.
Proving Your Impact and Ensuring Sustainability
To keep your nutrition education programs funded, you must prove they work. This means going beyond simple metrics like attendance. For long-term sustainability, you need a data-driven way to show clear, measurable value to payers, leadership, and community stakeholders.
https://www.youtube.com/embed/lvl5oizfobM
The goal is to connect your program’s activities to the outcomes healthcare organizations care about: better health, lower costs, and higher quality of care. It’s about building an undeniable business case.
Focusing on Metrics That Matter
Vanity metrics don’t tell the full story. True impact is measured by tracking the clinical and financial data that reflects improved patient health and less strain on the healthcare system.
Your measurement framework should zero in on:
- Clinical Biomarkers: Quantifiable changes in key health stats, like A1c levels for patients with diabetes, blood pressure readings, or cholesterol levels.
- Healthcare Utilization: Track a drop in expensive interactions, like fewer emergency room visits, lower hospital readmission rates, and less reliance on high-cost medications.
- Patient-Reported Outcomes (PROs): Capture the patient’s own perspective on their health, quality of life, and ability to manage their condition.
This focus shifts the conversation from “how many people we served” to “how much we improved health and saved money”—a language that resonates with payers and executives.
The Power of Qualitative Feedback
Hard data is crucial, but it doesn’t capture the human side of success. Pairing quantitative metrics with powerful, real-life feedback creates a richer, more persuasive narrative. This is where your CHWs are invaluable. Their regular check-ins provide on-the-ground insights into a patient’s progress, struggles, and personal victories.
Umoja Tip: We build simple, standardized reporting templates for our CHW partners to capture key observations after each patient interaction. These structured notes make it easy to spot recurring themes and pull compelling testimonials that show the program’s real-world impact beyond the clinical data.
These stories—a patient who has enough energy to play with their grandkids, or another who finally understands how to read a nutrition label—are what make your impact reports memorable and deeply human.
Building the Case for Long-Term Investment
Sustainability comes from proving a clear return on investment (ROI). You must draw a straight line from your program’s outcomes to the strategic goals of your healthcare partners, whether that’s hitting value-based care initiatives or quality improvement targets.
The link between providing nutritious food and teaching people about it is a powerful model. School meal programs have understood this for years. In 2022, 37% of these global programs included a nutrition education objective because providing food is only half the battle.
Your program’s success hinges on showing how it contributes to the bigger picture. When you can present a dashboard showing a 15% reduction in ER visits among your participants, you’re not just discussing a successful nutrition program; you’re presenting a direct cost-savings strategy. This transforms your program from a line-item expense into an indispensable clinical asset.
Your Top Questions About Nutrition Programs, Answered
When launching a nutrition education program in a healthcare setting, the practical, on-the-ground questions often determine success. This isn’t just a checklist; it’s a field guide built from real-world launches, covering CHW curriculum, telehealth adaptation, and the nitty-gritty logistics of food access.
What Should Our CHW Curriculum Actually Teach?
The secret is to shift the focus from reciting nutritional facts to building genuine coaching and motivational skills. A great CHW doesn’t just inform; they empower.
Your curriculum needs to stand on three pillars:
- Motivational Interviewing: Train CHWs to be fantastic listeners who help patients find their own reasons to change. This is infinitely more powerful than just telling someone what to do.
- Cultural Competency: Education must connect with lived experiences. Create materials reflecting local grocery stores, cultural dietary staples, and different levels of health literacy.
- Practical Tools: Give CHWs things they can use in the field, like “shoppable” grocery guides organized by aisle or simple, visual aids for portion sizes. Role-playing tough conversations is also a must-have.
How Do We Keep People Engaged with Telehealth?
Success with telehealth isn’t just about video calls. It’s about using multiple channels to ensure you’re not leaving anyone behind because of the digital divide.
A “no-tech to low-tech” philosophy has been a game-changer for our partners. For every digital tool you introduce, like a web-based meal planner, you need an analog version—like a printable, mail-out guide. This ensures a patient’s access to care never depends on their access to technology.
Build out a flexible communication strategy:
- Text-Based Nudges: Simple, automated messages work wonders for reminders, recipe ideas, or encouragement.
- Phone-Based Coaching: For patients uncomfortable with video, one-on-one calls provide truly personal support.
- Mail-Out Resources: High-quality printed materials like recipe cards and newsletters are essential for reinforcing learning offline.
How Do We Nail Down the Program Logistics?
Organizations want to know the best way to manage the operational side of food access. Whether you land on a pick-up or delivery model, the entire process must feel seamless and respectful.
Start by building food insecurity screening right into your clinical intake using a validated tool like the Hunger Vital Sign™. When it’s time for distribution, a hybrid model is often most effective. Offer a central pick-up location to foster community, but reserve delivery for your most vulnerable or geographically isolated participants.
A successful program isn’t just measured by the quality of your education. It’s about making the entire experience accessible, supportive, and dignified from the very first interaction.
Ready to launch a nutrition program that delivers real results? Umoja Health specializes in creating culturally connected, compliant Food is Medicine and nutrition security programs for healthcare partners nationwide. Explore our solutions today.