At their core, OAA compliant meal programs are federally funded initiatives born from the Older Americans Act (OAA). Their purpose is to deliver nutritious meals and vital supportive services to adults aged 60 and older.
These programs are the backbone of community nutrition for seniors, operating through both congregate (group) settings and home-delivered services. The goal is straightforward but critical: reduce food insecurity, head off malnutrition, and push back against the social isolation that too many older adults face.
Understanding The Older Americans Act Nutrition Program

The Older Americans Act Nutrition Program is a lifeline. It's one of the most essential community-based supports we have for older adults, providing a very real defense against hunger and loneliness. Its primary mission is to guarantee that seniors have consistent access to healthy food, which is fundamental to maintaining their health and living independently.
By offering meals in different formats—group settings for social connection and home delivery for those who are homebound—the program meets seniors where they are.
Since its creation in 1972, the OAA Nutrition Program has grown into the largest federally backed nutrition effort for older adults in the country. To give you a sense of scale, in 2020 alone, it provided roughly 198.6 million meals to more than 1.4 million seniors. That year saw a major spike, largely driven by the demands of the COVID-19 pandemic. For a deeper dive into the numbers and the program's reach, you can check out this detailed report on senior nutrition.
For anyone running one of these programs, it helps to have a quick reference for the main compliance pillars. This table breaks down the essentials.
Key OAA Requirements Breakdown
| Requirement Category | Specific Mandate | Purpose and Rationale |
|---|---|---|
| Nutritional Standards | Meals must provide a minimum of one-third of the Dietary Reference Intakes (DRIs) and comply with the Dietary Guidelines for Americans (DGAs). | To ensure meals are scientifically formulated to combat malnutrition, support chronic disease management, and promote overall health in older adults. |
| Participant Eligibility | Services are targeted to adults aged 60 and older. Programs must prioritize serving those with the greatest economic or social need. | To direct finite resources toward the most vulnerable populations, including low-income, minority, rural, and socially isolated seniors. |
| Service Delivery | Programs must offer meals through congregate settings, home-delivery, or both. They must also provide nutrition screening, education, and counseling. | To offer flexible access to meals while addressing the root causes of poor nutrition through education and preventative health screenings. |
| Fiscal & Reporting | Maintain auditable financial records, collect standardized participant data, and submit annual State Performance Reports (SPRs). | To ensure accountability for federal funds, demonstrate program impact, and allow for national-level analysis and oversight by the Administration for Community Living (ACL). |
Ultimately, these requirements work together to ensure that every meal served is part of a larger strategy to support senior independence and well-being.
Core Objectives of OAA Meal Programs
To fulfill its mission, the program is built around a few key objectives. These are the guideposts that direct how providers design and run their services, creating a consistent and effective support system across the nation.
- Reduce Food Insecurity and Malnutrition: The most direct goal is to provide meals that meet one-third of the Dietary Reference Intakes (DRIs), which directly improves a senior's nutritional status.
- Promote Health and Well-being: Programs are expected to offer nutrition screening, practical education, and counseling to help older adults manage chronic conditions and stay healthy.
- Decrease Social Isolation: Congregate meal sites are designed to be hubs for social interaction, giving seniors a chance to connect with peers and build community ties.
A core tenet of OAA compliant meal programs is that they deliver "more than just a meal." These programs act as crucial gateways to other essential services, like health screenings, wellness activities, and help with public benefits.
The Two Primary Service Models
OAA meal programs generally operate using two distinct but complementary models to serve a wide range of seniors with different needs.
Congregate Meals are served in group settings such as senior centers, community buildings, or churches. This model is all about fostering social connection and creating a supportive community atmosphere to go along with a healthy meal.
Home-Delivered Meals are for individuals who can't leave their homes easily due to illness, disability, or mobility issues. This service is absolutely essential for making sure isolated seniors not only get regular, healthy food but also a friendly wellness check from the person delivering the meal.
Navigating Key OAA Legal and Regulatory Requirements
Successfully running an OAA-compliant meal program really boils down to having a rock-solid grasp of the legal and regulatory rules of the road. This isn't just about checking boxes; following these rules is a core requirement for getting federal funding and, just as importantly, making sure your program has integrity. These regulations are in place for a good reason—to guarantee that the services we all provide are effective, fair, and accountable.
The rules cover just about everything, from who can get a meal to the precise nutritional breakdown of the food on the plate. This framework is what ensures every provider, no matter where they are, is meeting a consistent, high standard of care for older adults.
Participant Eligibility and Targeting
At its heart, the OAA is laser-focused on serving adults aged 60 and older. But true compliance goes deeper than just checking an ID. The Act specifically requires that programs prioritize serving seniors with the greatest economic or social need, putting a spotlight on certain vulnerable groups.
This targeted approach makes sure that our limited resources get to the people who are struggling the most. As an operator, this means you need to have systems in place that can actually identify and reach these populations. For organizations looking to get their government-funded programs running smoothly, Umoja Health offers practical guidance on how to scale compliant programs.
Key populations that need to be at the front of the line include:
- Low-income individuals, especially those living below the poverty line.
- Minority older adults, who often face systemic hurdles in accessing services.
- Seniors in rural communities, where support can be hard to come by.
- Those with limited English proficiency.
- Individuals at risk of being placed in an institution.
Nutritional Standards and Program Mandates
The nutritional requirements for OAA meals are exact and there’s no room for negotiation. Every single meal has to be built to meet the Dietary Guidelines for Americans (DGAs) and deliver a minimum of one-third of the Dietary Reference Intakes (DRIs) for older adults. This isn't arbitrary; this scientific standard is what makes these meals such a powerful weapon against malnutrition.
But it’s not just about the food. The OAA also lays out several other mandatory parts of the program. These elements work together to create a support system that addresses the whole person, not just their hunger.
The OAA demands more than just a meal delivery service; it mandates a complete service model. This includes things like nutrition screening to catch at-risk seniors early, education to help people make healthier choices, and rigorous fiscal management to ensure every dollar is used wisely.
Compliance also stretches into the back office. Program operators have to maintain strict confidentiality for participants, follow specific data collection rules, and make sure all their financial practices are transparent and ready for an audit at any time. These legal and regulatory guardrails are absolutely essential for maintaining the trust and effectiveness of OAA compliant meal programs across the country.
Case Study: Umoja's Path to OAA Compliance

This section provides a documentation-style overview of Umoja's transition from a general food distributor to a specialized provider of OAA compliant meal programs. The objective was to build a scalable, audit-ready nutrition program that exceeded baseline federal standards. This required strategic planning, subject matter expertise, and a robust data management infrastructure.
The Compliance Implementation Timeline
Umoja’s transition was structured into four distinct phases, each with specific objectives and deliverables. This phased approach ensured a solid foundation before scaling, minimizing risk and costly rework.
-
Phase 1: Needs Analysis and Strategic Planning (Months 1-2):
- Objective: Define the gap between current capabilities and OAA requirements.
- Activities: Conducted a comprehensive gap analysis. Secured initial funding. Assembled a core project team, including a registered dietitian (RD) and a compliance officer.
- Deliverable: A detailed Project Implementation Plan, including budget, risk assessment, and key performance indicators (KPIs).
-
Phase 2: System Development and Menu Architecture (Months 3-5):
- Objective: Build the operational and nutritional framework for compliance.
- Activities: The RD developed a four-week cyclical menu meeting the one-third DRI standard. The IT team designed and implemented a data collection system to track participant intake, nutritional risk scores, and meal delivery confirmations.
- Deliverable: Approved cyclical menus with full nutritional analysis; a functional, tested participant data management system.
Lesson Learned: Front-Load Dietitian Expertise. Engaging a registered dietitian with OAA experience during Phase 1 was critical. Their expertise in therapeutic diets and cultural adaptations prevented weeks of menu revisions. A common error is designing menus first and seeking RD approval later, which invariably leads to significant rework.
-
Phase 3: Pilot Program and Supply Chain Validation (Months 6-8):
- Objective: Test all systems and logistics in a controlled environment.
- Activities: Launched a limited pilot program with 50 participants. This allowed for stress-testing of delivery logistics, data collection workflows, and supply chain integrity. Simulated supply chain disruptions were conducted to validate backup vendor protocols.
- Deliverable: A Pilot Program Assessment Report detailing operational efficiencies, challenges, and recommended adjustments for full-scale launch.
-
Phase 4: Full-Scale Launch and Continuous Improvement (Month 9 Onward):
- Objective: Roll out the program to the full service area and establish an ongoing optimization process.
- Activities: Expanded the program based on pilot findings. Implemented a continuous improvement loop using monthly performance data and participant satisfaction surveys to refine menus and delivery operations.
- Deliverable: A fully operational OAA compliant meal program with an established monthly and quarterly review cadence.
Overcoming Operational Challenges
Umoja encountered several real-world challenges during implementation. A key supply chain disruption occurred when a primary vendor for low-sodium vegetable stock failed to deliver. Due to proactive sourcing and vetting of secondary and tertiary suppliers in Phase 3, the team was able to pivot to a backup vendor within 48 hours, preventing any interruption in meal service. This underscored the necessity of building procurement redundancy from the project's outset.
Another challenge was accommodating the diverse dietary needs of the initial participant cohort, which included requests for renal-friendly, vegetarian, and culturally specific Hispanic meals. Instead of creating dozens of unique menus, Umoja developed a modular menu system. This involved standardizing core components (e.g., protein, grain) and creating pre-approved substitution lists for sides and seasonings, enabling efficient kitting while respecting individual requirements. This structured flexibility became a cornerstone of their successful OAA compliant meal programs.
OAA Documentation: The Compliance Blueprint
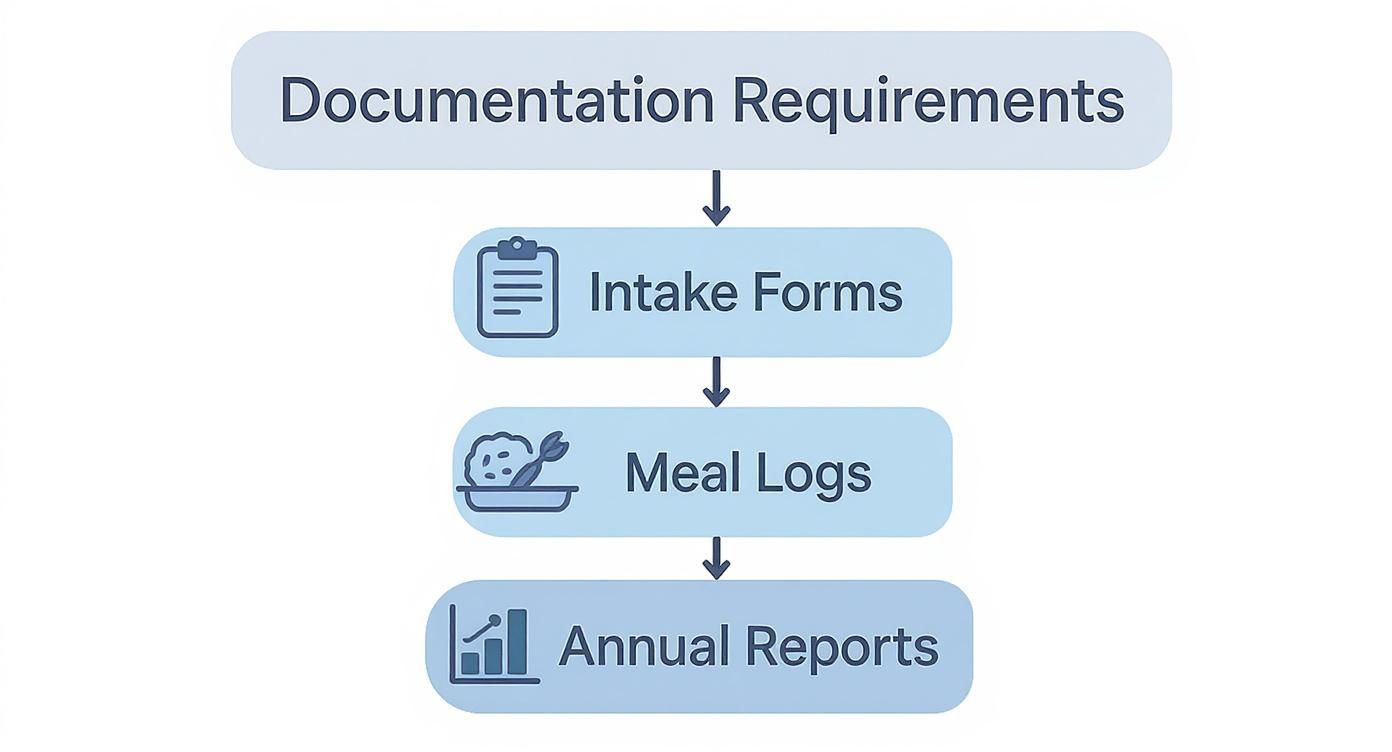
For OAA compliant meal programs, documentation is the definitive record of compliance. It serves as the primary evidence for audits, justifies funding, and provides the data necessary for continuous program improvement. This section outlines the essential documentation required to maintain program integrity.
Required Documentation for Daily Operations
Meticulous daily record-keeping is non-negotiable for proving compliance with operational and service standards. The following documents form the backbone of an audit-ready program.
- Participant Intake Forms: This initial record must capture all data necessary to establish eligibility (age 60+), demographic information for reporting, and self-disclosed needs to ensure targeting requirements are met.
- Nutritional Risk Assessments: Programs are required to screen participants for nutritional risk at intake and at regular intervals thereafter, often using a standardized tool like the DETERMINE checklist. These records are crucial for identifying at-risk individuals for targeted intervention and for reporting on health outcomes.
- Meal Service and Delivery Logs: Daily logs must be maintained to track every meal served. For congregate sites, this is a sign-in sheet. For home-delivered routes, this is a driver log. These logs are the source data for reimbursement and service reporting.
- Food Safety and Temperature Logs: To comply with food safety regulations, daily logs must record the temperatures of food at critical control points: cooking, holding, transport, and delivery. This documentation is essential for preventing foodborne illness and demonstrating due diligence.
To an auditor, undocumented action is equivalent to action not taken. Clear, consistent, and complete documentation is the ultimate proof of adherence to federal safety, eligibility, and service mandates.
Data Requirements for State Performance Reports
All daily operational data culminates in the annual State Performance Report (SPR), a mandatory submission to the Administration for Community Living (ACL). This report provides a national overview of the OAA Nutrition Program's reach and impact.
Data systems must be configured to capture and aggregate the specific metrics required by the SPR.
Key data points that must be tracked for the SPR include:
- Unduplicated Participant Count: The total number of unique individuals served during the reporting year.
- Total Meal Counts: Aggregated totals for both congregate and home-delivered meals provided.
- Targeted Population Demographics: Detailed breakdowns of participants by age, gender, race/ethnicity, income level, and rural status to demonstrate service to vulnerable populations.
- Nutritional Risk Status: Aggregated data from nutritional risk assessments, showing the percentage of participants at high nutritional risk.
Failure to produce accurate SPR data can jeopardize state funding and indicates a fundamental weakness in program management. A well-designed data system transforms this requirement from an annual crisis into a routine report.
Operational Checklists for Program Integrity
Keeping an OAA-compliant meal program running smoothly means every single partner knows exactly what their role is. When food banks, state agencies, MCOs, and 3PL partners are all on the same page, upholding federal standards becomes second nature. These checklists are designed to be quick, practical references to keep collaboration tight and ensure compliance across the entire network.
Think of these as your go-to guides, broken down by the core duties of each key player.
For Food Banks and Community-Based Organizations
Food banks and CBOs are the heart of the operation—the ones on the front lines handling meal prep and getting food to participants. For them, it's all about food safety, keeping track of inventory, and interacting directly with seniors.
- Inventory Management: You need a solid system for tracking your stock of OAA-compliant components. This means constantly monitoring expiration dates and making sure allergens are properly segregated to keep everyone safe.
- Volunteer Training: Your volunteers are invaluable, so consistent training is a must. Cover the essentials: safe food handling, sticking to portion control guidelines, and, of course, the importance of client confidentiality.
- Documentation: If it isn't written down, it didn't happen. Maintain daily logs for meal production counts, food temperatures, and distribution records. This isn't just busywork; it's what keeps you audit-ready at all times.
For State Agencies on Aging
State Units on Aging (SUAs) and Area Agencies on Aging (AAAs) have the big-picture view. They're in charge of oversight, managing the funding, and making sure every part of the program is compliant.
- Monitoring and Oversight: It’s vital to get out in the field. Schedule regular site visits with your local providers to do a thorough review of their meal service operations, check their documentation, and observe their food safety practices firsthand.
- Fiscal Accountability: The money has to be right. Verify that every expenditure lines up with OAA funding rules and that all providers are keeping meticulous financial records for reporting.
- Data Reporting: Good data is the foundation of a strong program. You're responsible for collecting, validating, and submitting accurate State Performance Report (SPR) data from all local providers straight to the Administration for Community Living (ACL).
For Managed Care and 3PL Partners
Managed Care Organizations (MCOs) and Third-Party Logistics (3PL) providers are critical links in the chain, handling referrals and the physical journey of each meal.
- MCO Client Referrals: Your process for referring eligible members to OAA meal programs has to be both secure and efficient. It's just as important to have a system to confirm that service has actually started for each person.
- 3PL Delivery Protocols: Route optimization is key, but so is maintaining strict temperature controls while meals are in transit. Drivers also play a unique role; they should be trained to perform quick wellness checks during home deliveries. And on the assembly side, an efficient workflow for scalable kitting can make a huge difference.
Getting the right equipment is fundamental to safety and efficiency. A good commercial kitchen equipment checklist isn't just a list—it's an invaluable tool for maintaining the operational integrity of your entire OAA-compliant meal program.
Your Questions About OAA Compliance, Answered
When you're running a meal program on the ground, the official guidelines can bring up a lot of practical questions. Here are some straight answers to the most common things we hear from operators.
Who Exactly Can Receive an OAA Meal?
The basic rule is simple: anyone 60 years of age or older is eligible.
While there are no income tests to get a meal, the Older Americans Act does require programs to focus their efforts on seniors with the greatest economic and social need. Think low-income individuals, minority seniors, folks in rural areas, and anyone at risk of being moved into an institution.
Are We Allowed to Charge for OAA Meals?
No, you can't ever charge a fee for an OAA meal. The rules are very clear on this.
What you are required to do is give every participant a chance to make a voluntary contribution toward the cost of their meal. This process has to be completely confidential, and every dollar brought in must be used to expand the meal service. Most importantly, no one can ever be denied a meal because they are unable or unwilling to contribute.
At its heart, the OAA sees these meals as a right, not something to be bought and sold. The voluntary contribution system helps programs bring in extra funds while still protecting the dignity of every single person you serve, no matter what their financial situation is.
How Should We Handle Complex Medical Diets?
This is a big one. Managing special diets for conditions like renal disease or dysphagia is a crucial part of staying compliant. The short answer is that programs must provide therapeutic meals when it's feasible and medically necessary. This isn't something you can eyeball; the entire process has to be managed by a registered dietitian (RD) who can formally approve and document the need for that modified diet.
For example, a low-sodium meal for someone with high blood pressure is a fairly common request that programs are expected to handle. But a more complex order, like a pureed, low-potassium diet, is a different story. That would demand a doctor's order and very careful planning with your RD to make sure the meal is safe, appropriate, and still meets all the core nutritional standards. It’s all about making sure every participant gets a meal that genuinely supports their health.
At Umoja Health, we live and breathe this stuff. We specialize in helping organizations run compliant programs at any scale. Whether it's developing OAA-compliant menus from scratch or providing shelf-stable meal kits that just work, we have the products and deep experience you need. Explore our solutions at https://umojahealth.com.

