Registered dietitian (RDN) meal programs aren’t just about handing out food; they’re structured, clinically-informed plans designed and overseen by certified RDNs. The goal is to tackle specific health challenges, help manage chronic diseases, or simply improve overall wellness by turning complex clinical guidelines into practical, ready-to-eat meals or multi-day kits. It’s about making medically appropriate nutrition accessible.
Laying the Groundwork for Your RDN Program
The very first thing you need is a clear vision. Who are you trying to help, and what does success look like for them? Nailing down the answers to these questions will be your North Star for every decision that follows, from what goes in the box to how you get reimbursed.
Defining Your Population and Program Goals
Start by getting laser-focused on the specific patient population you’ll serve. Are you working with individuals just diagnosed with Type 2 diabetes? Maybe it’s seniors facing food insecurity, or families navigating the WIC program. Each of these groups has a completely different set of needs, cultural food preferences, and real-world logistical challenges.
Once your “who” is clear, you need to set SMART goals—that’s Specific, Measurable, Achievable, Relevant, and Time-bound. Vague ideas like “improve health” won’t cut it. You need concrete targets that prove your program is working.
Think more along these lines:
- Reduce A1c levels by an average of 1% over a 12-week period for participants with diabetes.
- Increase fruit and vegetable consumption by two servings per day among enrolled families.
- Decrease hospital readmission rates for congestive heart failure patients by 15% within six months.
These are the kinds of hard numbers that demonstrate value to healthcare partners, funders, and anyone else who needs to see a return on investment. At Umoja, our “Food as Medicine” programs are built around these kinds of clear clinical endpoints. It’s a major reason we’re able to build strong partnerships with managed care organizations focused on value-based care.
Structuring Your Program Model
With your population and goals locked in, you can choose the right program model. So-called ‘Food is Medicine’ initiatives, for instance, often focus on providing medically tailored groceries or fully prepared meals to patients with specific chronic conditions. These are almost always prescribed by a clinician and have direct RDN oversight.
Another really powerful approach is using specialized multi-day kits. We’ve found these to be incredibly effective for public health programs like CACFP, SFSP, or WIC pilots. By bundling compliant food items for several days, you simplify distribution and ensure families have a consistent supply of nutritious food. If you want to see how we put these together, you can dig into our guide on comprehensive kitting programs.
A key Umoja best practice is co-designing programs with the community. Before finalizing menus or materials, we conduct focus groups with potential participants to ensure the food is culturally connected and the program design respects their lived experiences. This builds trust and boosts engagement from day one.
Designing Medically Tailored and Engaging Menus

Here’s where the art and science of a successful dietitian-led meal program really come together. You have to walk a fine line: design meals that meet strict medical guidelines while also being delicious, appealing, and culturally connected to the people you serve. If the food doesn’t resonate, it doesn’t matter how clinically perfect the menu is—it just won’t work.
This is where RDNs shift from scientist to craftsperson, turning therapeutic dietary needs into meals that patients genuinely look forward to eating. That blend of precision and creativity is the secret sauce for patient satisfaction and, ultimately, program adherence.
Building Menus From the Component Level Up
When you’re creating multi-day kits or meal plans, you have to get granular. It all starts with defining detailed component specifications. In plain English, that means breaking down every single meal into its individual parts and setting crystal-clear standards for each one.
A “heart-healthy” meal kit, for instance, isn’t just a random box of low-sodium foods. A dietitian needs to specify the exact components:
- Protein: 4 oz. skinless chicken breast, baked not fried, with sodium under 200mg per serving.
- Starch: 1 cup cooked brown rice, specifically long-grain for texture.
- Vegetable: 1.5 cups steamed broccoli florets, fresh or frozen, with no added salt or butter.
- Fruit: One medium apple, sourced from a U.S. grower to meet compliance standards.
This level of detail is absolutely critical for consistency, nutritional accuracy, and procurement. It guarantees that every kit going out the door meets the prescribed medical nutrition therapy guidelines, no matter who’s on the assembly line. Plus, these specs are essential for managing costs and inventory with your suppliers.
Navigating Compliance and Sourcing
If your program serves specific populations, like students in school lunch programs, you’ll run into another layer of rules. One of the biggest is the Buy American provision, which requires schools to buy domestically grown and processed foods whenever possible.
This means your sourcing strategy has to put U.S. producers first. An RDN designing menus for an SFSP or CACFP program has to work hand-in-glove with procurement teams to verify the origin of every single component—from the flour in the tortillas to the fruit in the snack packs. Building strong relationships with local and regional suppliers isn’t just a good idea; it’s a key strategy for a compliant and resilient supply chain.
The best menus are co-created. At Umoja, we regularly hold taste-testing sessions with community members to get their direct feedback. We’ve adjusted spice levels, swapped out ingredients, and even redesigned entire meals based on what they tell us. That input dramatically improves program buy-in.
Managing Costs With Smart Procurement
Ingredient costs can swing wildly, and that can put your program’s budget at serious risk. The best defense is a good offense: forward-buying. This simply means purchasing key ingredients in bulk when prices are low to lock in savings for the future.
This strategy works especially well for the shelf-stable items that are the backbone of so many multi-day kits:
- Canned beans and vegetables
- Rice, pasta, and other whole grains
- Shelf-stable milk and plant-based alternatives
- Nuts, seeds, and dried fruit
By keeping an eye on market trends and forecasting needs, RDNs and supply chain managers can make strategic buys that protect the program from price spikes. This creates cost stability and allows the program to serve more people without ever skimping on quality. It’s a core part of effective Food is Medicine initiatives.
Kitting Workflows and Food Safety
Once the ingredients are sourced, the kitting process has to be absolutely flawless. Designing an efficient and safe assembly workflow is non-negotiable. The flow should be set up to minimize any risk of cross-contamination, especially with allergens, and maintain strict temperature controls for cold-chain items.
A well-designed kitting station might have designated zones for dry goods, refrigerated items, and frozen components. Your Standard Operating Procedures (SOPs) should clearly map out every step, from handwashing protocols to the precise order of packing. Food safety has to be built into the process, not treated as an afterthought. This operational discipline ensures that every medically tailored meal arrives at a patient’s home safe and ready to support their health.
This focus on the individual is driving major changes in the industry. The personalized nutrition market is projected to reach USD 82.66 billion by 2035, fueled by technologies that allow dietitians to create highly specific meal plans.
Mastering Logistics From Procurement to Delivery
A brilliant, medically tailored menu is only half the battle. If that food doesn’t reach the patient safely, on time, and in perfect condition, the clinical work is all for nothing. This is where the operational side of a meal program truly shines—or fails. Mastering the logistics, from sourcing ingredients all the way to that final knock on the door, is absolutely non-negotiable for building a program people can trust.
This isn’t just about packing a box. It’s about a rock-solid strategy for procurement, an unwavering commitment to food safety through cold chain management, and a patient-first approach to the final delivery. Get these pieces right, and you create a seamless experience that reinforces the care and quality baked into your entire program.
Building a Resilient Supply Chain
Strong, reliable supplier relationships are the bedrock of any successful meal program. You need partners who get your exacting standards for quality, nutritional content, and compliance—like the Buy American provision. Don’t just hunt for the lowest price. Look for partners who can guarantee consistency and give you transparency into their sourcing.
One of the smartest ways to manage your budget and lock in a steady supply of key ingredients is forward-buying. This simply means purchasing non-perishable staples in bulk when the market prices are in your favor.
- What to Forward-Buy: Think shelf-stable items. We’re talking whole grains like brown rice and quinoa, legumes like canned beans and lentils, and other pantry essentials that form the base of your kits.
- When to Buy: Work with your procurement team to watch market trends. Buying off-season or in larger quantities can lock in significant savings that shield your program from surprise price hikes down the road.
This proactive approach to procurement gives you the stability you need to scale up without ever compromising the quality or affordability of your meals.
Mastering the Cold Chain
Maintaining the cold chain is, without a doubt, one of the most critical operational challenges you’ll face. This is the uninterrupted series of refrigerated production, storage, and distribution activities that keeps food safe. A single failure here can destroy patient trust in an instant.
Success requires a layered approach that pulls together technology, the right materials, and clear protocols for when things inevitably go wrong.
A common exception we plan for is a “failed delivery attempt,” where a patient isn’t home. Our standard operating procedure (SOP) is for the driver to immediately return the temperature-sensitive kit to a refrigerated hub. The kit is never left on a doorstep, ensuring the cold chain is never broken.
Here are the key components of a robust cold chain:
- Temperature Monitoring: Using data loggers inside shipments gives you a continuous record of the internal temperature. This is your proof that safety standards were met all the way from your facility to the patient’s door.
- Validated Packaging: Don’t skimp here. Invest in insulated liners and correctly sized cold packs that have been tested to hold safe temperatures (below 41°F) for much longer than your maximum expected delivery time.
- Handling Exceptions: Create simple, actionable plans for every possible snag, from a vehicle breakdown to a patient not answering the door. Your drivers need to be empowered with the knowledge and tools to make the right call every time.
This journey—from sourcing to a safe delivery—is a chain where every link matters.
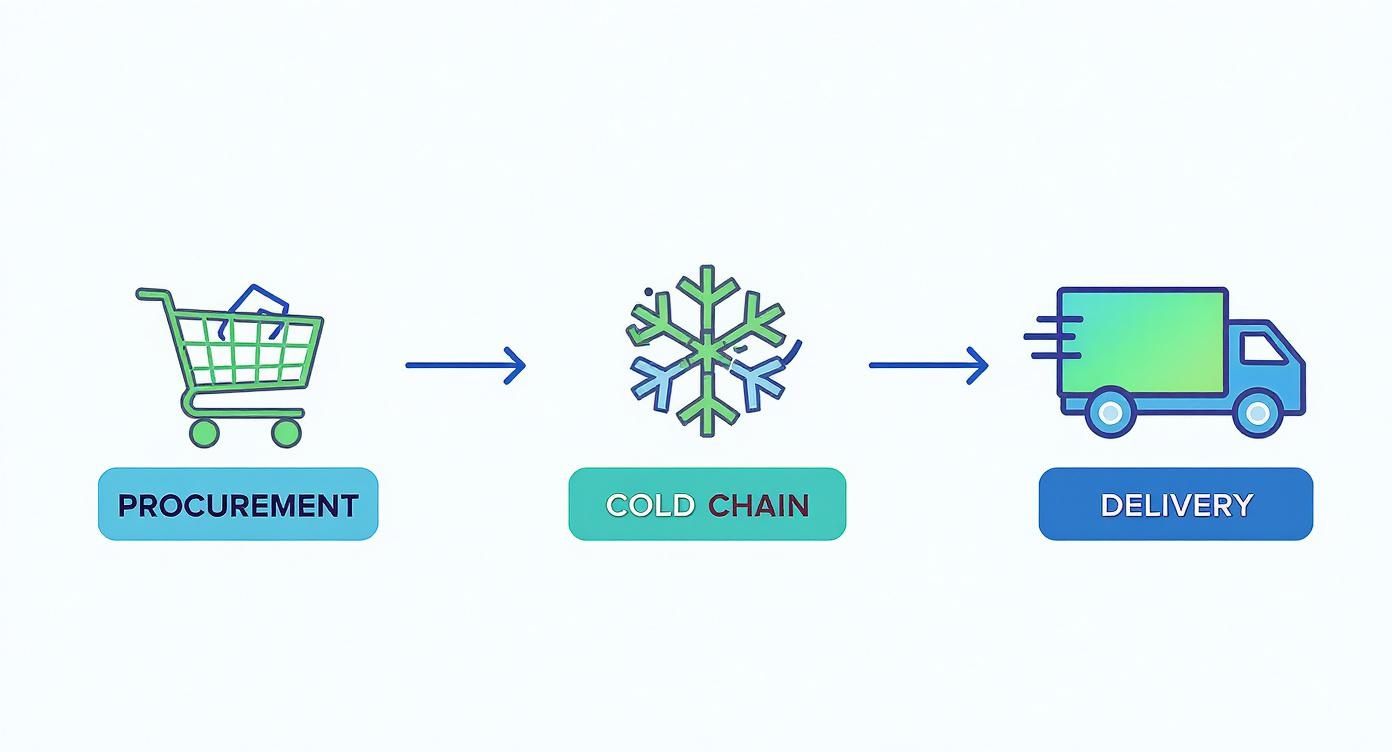
As the visual shows, these stages are completely interconnected. A failure in one step compromises the whole system.
Optimizing the Final Mile
The final delivery is your program’s last touchpoint. It’s your last chance to make a great impression. An optimized delivery workflow isn’t just about speed; it’s about creating a reliable and reassuring experience for the people you serve.
This starts with smart routing and scheduling to create predictable delivery windows. When you communicate those windows clearly to patients, you reduce their anxiety and cut down on missed deliveries. Just as important are professional, courteous drivers who understand the sensitive nature of what they’re carrying—they’re invaluable assets.
For organizations looking to manage these complex workflows, exploring specialized food-grade logistics solutions can provide the infrastructure and expertise to ensure everything runs smoothly and stays compliant. A seamless final mile solidifies a patient’s confidence in the quality of your entire program.
Mapping the Patient Referral and Engagement Journey

You can have the most meticulously designed menu and flawless logistics, but none of it matters if patients don’t actually enroll and stay the course. The journey from a clinical referral to an engaged, successful participant isn’t accidental. It requires a thoughtful, human-centered approach.
It’s really about building a supportive pathway that makes it easy for patients to say “yes” and feel motivated from the very first interaction. That process begins long before the first meal kit arrives on their doorstep. It starts with a clear, seamless referral system that builds trust with your clinical partners and cuts down on the friction for patients who are often juggling complex health challenges.
Designing the Referral and Onboarding Workflow
The handoff from a healthcare provider to your registered dietitian meal program is a make-or-break moment. A clunky or confusing process can cause potential participants to drop off before they even start. A smooth workflow, on the other hand, signals professionalism and care, setting a positive tone for the entire experience.
You need to map out the entire journey with clear steps and designated responsibilities. This ensures everyone, from the referring physician’s office to your intake coordinator, knows their exact role and what comes next.
Here’s a look at how we map the patient journey. It’s a simple but powerful tool for keeping everyone aligned and ensuring no patient feels lost in the process.
Patient Referral Journey Map
| Stage | Key Action | Responsible Party | Umoja’s Best Practice |
|---|---|---|---|
| Referral | Physician submits a secure referral with patient diagnosis and dietary needs. | Referring Provider | Use a simple, HIPAA-compliant digital form that takes less than two minutes to complete. |
| Initial Contact | Program staff contacts the patient within 24-48 hours to introduce the program. | Intake Coordinator | Lead with empathy. The goal is to build rapport, not just verify information. |
| Onboarding | RDN conducts an initial assessment, confirms eligibility, and explains the program. | Registered Dietitian | Frame the program as a partnership. Use this call to set collaborative health goals with the patient. |
| Activation | Patient provides consent, and their first meal delivery is scheduled. | Program Administrator | Send a welcome email or text immediately after the call, confirming the start date and what to expect. |
Having a structured approach like this ensures no one falls through the cracks. More importantly, it helps every patient feel seen and supported from day one.
The First Conversation: A Model Engagement Script
That initial call is your single best opportunity to build trust and motivate a new participant. Think of it less as an intake and more as an invitation. The script shouldn’t feel robotic. It’s a guide for a natural conversation that uncovers the patient’s real motivations and addresses their concerns head-on.
Here’s a model script structure we’ve seen work wonders, which you can adapt for your own registered dietitian meal program.
RDN: “Hi, [Patient Name]. My name is [Your Name], and I’m a registered dietitian with the [Program Name] program. Your doctor, [Doctor’s Name], referred you because they believe our program could be a great support for your health goals. How are you feeling today?”
(Just pause and listen. This acknowledges them as a person, not just a referral on a list.)
RDN: “I’d love to tell you a bit about how we partner with patients. Essentially, we provide delicious, ready-to-use meal kits designed specifically to help with [Patient’s Condition, e.g., managing blood sugar]. Our goal is to make healthy eating easier and less stressful for you. Does that sound like something that might be helpful?”
(This frames the benefit directly to them and connects the program to their immediate needs.)
RDN: “Many people we work with find that having these meals on hand gives them more time and energy. Before we go further, what’s the biggest challenge you face right now when it comes to food and meals?”
(This simple question opens the door for them to share their story, turning a one-way call into a collaborative session.)
The secret ingredient here is active listening. The script provides a framework, but the patient’s own answers should guide where the conversation goes. Your goal is for them to hang up feeling heard and understood—that’s the foundation of a strong therapeutic alliance.
Creating Lasting Engagement
Engagement doesn’t stop after the first delivery. It has to be woven into the fabric of the entire program. We do this through consistent, supportive communication and practical educational materials that empower patients for the long haul.
Consider weaving these elements into your program:
- Weekly Check-in Texts: A simple, automated message asking “How are you enjoying the meals this week?” can make a huge difference in making someone feel cared for.
- Simple Educational Materials: Slip a one-page handout into each delivery with a tip of the week, like “How to Read a Nutrition Label” or “Tips for Healthy Snacking.” Keep it simple and actionable.
- RDN Accessibility: Offer brief, scheduled follow-up calls to answer questions, troubleshoot challenges, and, most importantly, celebrate their small wins.
By building this supportive ecosystem, you transform a meal delivery service into a comprehensive care program. That’s how you encourage adherence and drive the lasting health outcomes you’re aiming for.
Accreditation, Billing, and Reimbursement
A brilliant program model can’t survive on passion alone. It needs a solid financial engine to have any lasting impact. For many RDNs, figuring out the money side of things—accreditation, billing codes, and reimbursement—is the most intimidating part of the process. This is where you build a financially sustainable program that can actually grow and serve more people.
Accreditation: Becoming a Recognized Provider
Before you can bill, you need to establish credibility with payers. This starts with gaining accreditation and becoming a recognized healthcare provider.
- Get an NPI Number: The first step is getting a National Provider Identifier (NPI). This is your unique identification number within the healthcare system, essential for all billing and administrative transactions.
- Get Credentialed: The next major hurdle is getting credentialed with insurance companies, including commercial payers, Medicare, and Medicaid. This involves a lengthy application process to prove you meet their standards of care, but it’s the key that unlocks the door to reimbursement.
Umoja’s best practice is to start the credentialing process months before you plan to launch. Having your NPI and being in-network with key local payers before you see your first patient will save you a world of administrative headaches.
Billing for Your Services
Once you’re credentialed, you can bill for your work using specific Current Procedural Terminology (CPT) codes. These five-digit codes are the universal language for telling insurers exactly what service you provided. For RDN-led nutrition programs, the core codes are for Medical Nutrition Therapy (MNT).
- 97802: For an initial MNT assessment, billed in 15-minute increments.
- 97803: For follow-up reassessments and interventions, also in 15-minute blocks.
- 97804: For group MNT sessions, covering 30 minutes per person.
Meticulous documentation is critical. Your notes must clearly link your nutrition counseling directly to the patient’s medical diagnosis, justifying the billing code and demonstrating the medical necessity of your program to get claims paid.
Building a Resilient Funding Strategy
Relying on a single income stream is risky. The most resilient programs build a diversified funding strategy, weaving together different payment models to create stability and open up more avenues for growth.
- Fee-for-Service: The traditional model where you conduct an MNT session, bill an insurer (like Medicare/Medicaid), and get paid.
- Value-Based Care Contracts: Increasingly common with Managed Care Organizations, these arrangements tie your payment to patient outcomes. For instance, a health plan might offer a bonus for hitting a target reduction in A1c levels across your diabetic patient population.
- Grant Funding: Community foundations, government agencies, and corporations offer grants for programs that tackle food insecurity, chronic disease, or health equity. These funds can be a lifeline for launching a pilot or expanding services to underserved communities.
By combining these different streams, you build a much stronger financial foundation, giving your program the breathing room it needs to truly thrive.
Proving Your Program Works: A Guide to Monitoring and Reporting
How can you be sure your meal program is making a real difference? The answer is in the data. A smart monitoring and reporting system is what turns anecdotal wins into hard evidence. It’s how you prove the value of your registered dietitian meal program to funders, healthcare partners, and the very community you serve.
This isn’t just about ticking boxes for accountability. It’s about building a compelling, data-backed story of your impact. By tracking the right numbers, you justify your program’s existence, secure ongoing support, and make a powerful case to grow.
What Should You Actually Measure? Identifying Your KPIs
To measure success, you first have to define what success looks like for your specific program. It comes down to picking a balanced mix of Key Performance Indicators (KPIs) that capture both the clinical results and the operational health of your initiative. These metrics should tie directly back to the goals you set in the design phase.
Your KPIs should fall into a few key categories:
- Clinical Outcomes: These are the hard health numbers. We’re talking A1c levels for diabetic patients, blood pressure readings, or shifts in cholesterol.
- Engagement Metrics: This is all about participation. How well are people sticking with the program? You can track adherence rates, the number of completed educational videos, or attendance at check-ins with the RDN.
- Patient-Reported Outcomes (PROs): Don’t forget to ask people how they feel. Simple surveys can capture powerful subjective data, like improvements in quality of life, a greater sense of food security, or more confidence in managing their health.
- Operational Metrics: These keep you efficient. Things like on-time delivery rates or the average cost-per-participant are critical for sustainability.
A rookie mistake is trying to track everything. Start with a handful of high-impact KPIs for each category. For a diabetes program, that might be A1c, the program adherence rate, and a simple quality-of-life survey score. You can always add more detail later.
Setting Up Systems to Capture the Data
Great data collection has to be simple for your team and non-intrusive for your patients. This is where modern tools are a huge help. The global market for dietitian software has exploded, valued at around $450 million in 2023 and projected to hit $870 million by 2032. Platforms now bundle patient management, meal planning, and reporting, which makes collecting and analyzing data much more efficient. You can get more market insights from the team at Dataintelo.com.
For clinical data, secure integrations with electronic health records (EHRs) can automate much of the work. For engagement and patient-reported data, simple tools like automated text surveys or brief online forms can get you high response rates without creating a burden for anyone.
Creating Reports That Tell a Story
Data is pretty useless if it just sits in a spreadsheet. The final, critical step is translating your numbers into a clear, concise report that actually communicates your program’s success to the people who need to see it. A good report doesn’t just list numbers; it weaves them into a narrative.
A simple yet powerful reporting template could look something like this:
- Executive Summary: A one-paragraph snapshot of the key achievements from the reporting period.
- KPI Dashboard: A visual look at your main metrics. Use charts and graphs to show trends over time.
- Key Wins & Success Stories: Zero in on a specific positive outcome. Pair the data with a brief, anonymized patient testimonial to bring it to life.
- Challenges & Action Plan: Be honest about what didn’t work. More importantly, outline the concrete steps you’re taking to improve.
This structured approach turns your data into a powerful tool for advocacy, helping you prove the undeniable impact your program is having.
At Umoja Health, we build compliant, data-driven registered dietitian meal programs that deliver measurable outcomes for healthcare plans, government agencies, and community organizations. Find out how we can help you design and scale your Food is Medicine initiative.

