Food For Health
The positive economic, medical, and social impact of maternal nutrition as an intervention
Food is essential medicine for pregnant women. As a society, we strongly desire for new mothers and their infants to enjoy healthy, prosperous lives. The foundational step in achieving this is food security and good nutrition — for both mother and baby.
Pregnant women are particularly vulnerable to negative health consequences arising from food insecurity; therefore, it is essential to keep these women and their families from going hungry. It is important to help prepare women and their bodies for the nutritional demands of pregnancy and breastfeeding — should the mother choose to do the latter.
Unfortunately, the typical American diet is heavy in fatty red meat, processed foods, and sweetened foods/beverages, so many expectant mothers have to overcome this nutrition-related socio-cultural barrier. Furthermore, because pregnancy disrupts normal lifestyle physiological patterns, the diets of pregnant women tend to be less healthy than those of otherwise similar non-pregnant women. As a consequence, the sad reality is that most American women do not meet the recommendations for healthful nutrition and weight either before, during, or after pregnancy.1 Nearly 2/3 of American women enter pregnancy overweight or even obese.2 There is a strong connection between maternal obesity, childhood obesity, and diabetes, which has longer term implications as we discuss in a following section.
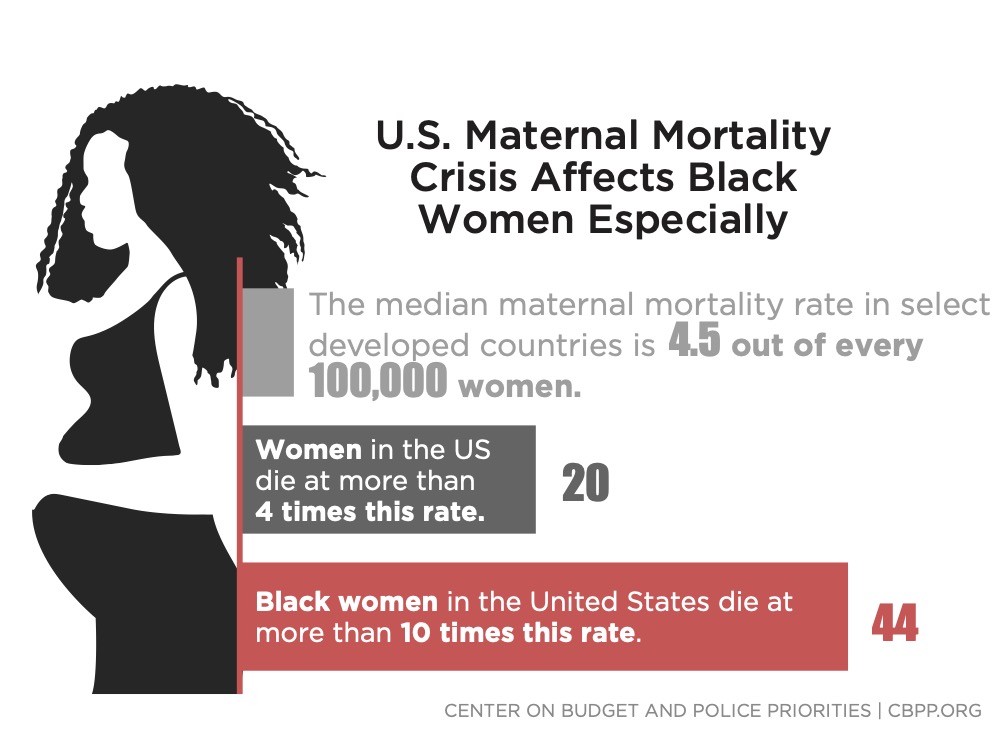
In large part because of this poor nutrition, the U.S. performs poorly on several maternity-related metrics. For example, compared to other advanced industrialized nations, the U.S. has the highest maternal mortality rate.3 While this has the potential to impact all socio-economic classes, the painful reality is that adverse maternity outcomes disproportionally impact the medically underserved. This includes people who are usually below the poverty line and often also (i) geographically distant from healthcare providers, (ii) lacking trust in clinicians, (iii) without access to native language providers, and (iv) without health insurance.
The advantages of getting maternal nutrition right are certainly important short-term but also have a high probability for extending well into the future. Gestation through early childhood is a highly predictive time for determining risks of chronic diseases for children as they mature into adults.4 The first days, weeks, months, and years for an infant and child provide the foundation for lifelong health — and disease. During this period, the external environments and internal food consumption shape the future health of children in enduring and powerful ways.
For example, excessive first trimester weight gains are a reliable predictor of later adverse outcomes.5 Maternal diets can cause profound, irreversible changes in the development, function, and structure of the infant’s bodily processes, key tissues, and vital organs (e.g., blood sugar, brain, immune system, kidney, liver, pancreas, and skeletal muscle). Consider type 2 diabetes mellitus, which has now reached epidemic proportions in certain U.S. subpopulations. During and immediately after birth, we should aim to prevent the immune cells programming for diabetes biologically in infants; this would interrupt the vicious downward cycle of diabetes across generations.
Positive and Negative Impacts of Nutrition on Mothers and Infants
During pregnancy, women experience increased nutritional demands to support changes in maternal tissues and metabolism, as well as fetal growth and development. Health-conscious food consumption before and during pregnancy leads to fewer medical complications.6 Relative to the pre-pregnancy period, a pregnant woman’s energy requirements increase by about 300 calores per day,7 and the need for proteins, minerals, and vitamins (e.g., calcium, folic acid iodine, iron, and zinc) grows significantly.8 Better nutrition for pregnant mothers translates into optimal fetal growth, improved perinatal survival, and overall short- and long-term health for the baby.
Breastfeeding provides an exemplar of the close connection between nutrition and health for both mother and infant. Because breast milk is uniquely suited to satisfy the nutritional needs of infants during the initial 4 to 6 months of life, breastfeeding by newborns can lower the risk of developing chronic diseases as adults. It can also have positive health benefits for mothers (e.g., reducing risk of developing type 2 diabetes). Additionally, breast milk can lower an infant’s risk of becoming obese later in life, and breastfeeding can reduce the mother’s risk of developing breast cancer, depression, diabetes, and ovarian cancer. When complications arise, optimal paripartum services can provide the additional support needed for mother and baby to achieve breastfeeding goals, reduce stress, improve postpartum mental health and ensure adequate nutrition for baby.
Conversely, there are several negative consequences attendant to the lack of access to nutritious food. Limited and uncertain access to nutritious food can be detrimental to mother and baby both during and after pregnancy. Either excessive or insufficient gestational weight gain, and pregnancy-related conditions such as gestational diabetes can lead to particularly adverse consequences. A nontrivial percentage of U.S. pregnancies are high-risk, often requiring cesarean section and NICU admissions,9 substantially increasing – often doubling the cost of delivery.
Substandard maternal nutritional status is associated with a range of unhealthy fetal growth patterns, including excessive size10, 11 and insufficient size.12 Key risk indications before and during pregnancy include abnormal/impaired glucose tolerance (i.e., gestational diabetes mellitus), cesarean delivery, gestational hypertension, longer hospital stay, preeclampsia, pregnancy-induced hypertension, preterm birth, obesity-related complications, and unsuccessful breastfeeding. Negative consequences for the fetus/infant include congenital defects, goiter, hypothyroidism, intellectual disabilities, low birth weight, neonatal asphyxia, preterm birth, stillbirth, stunting, and wasting.
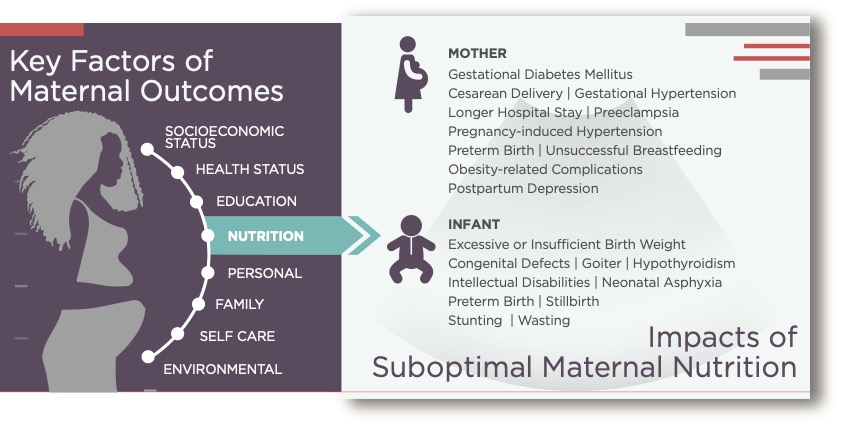
Poor diet and food insecurity can have other negative consequences. Food insecurity can increase the release of stress hormones that have been conclusively linked to a baby’s preterm birth and a mother’s unhealthy changes in pregnancy weight.13 Moreover, maternal diet is a significant determinant in the development of the gut microbiome, and the establishment of gut flora is essential to the health of an adult, including proper functioning of the gastrointestinal tract. The negative consequences also extend to mental health. Food insecurity can increase the probability of postpartum depression,14 and negatively impacts a pregnant mother’s blood pressure as well as other key health indicators.
Disparities, Inequity, and DEI Dimensions
As part of tackling food insecurity and poor nutrition relative to pregnancy, we also need to address implicit bias and health-related social barriers as these can cause and compound nutritional problems. Women of color all too frequently receive suboptimal care because of implicit biases based on gender and race/ethnicity. Particularly from the perspective of women and babies of color, the U.S. is experiencing a maternal and infant health crisis of dire proportions. Black women experience a 50% higher probability of preterm births than women of other races/ethnicities, and they are about 4 times more likely to die from pregnancy or childbirth-related complications.16, 17 Black infants are 2 times more likely to die than white infants.18
Because of this exceptionally poor track record and history of discrimination, many Black women experience apprehension, fear, and frustration regarding childbirth.19 Female Black, Indigenous, and people of color (BIPOC) often highlight gaps in communications when they are receiving peripartum care.20 This lowers their sense of autonomy in the care decision-making process. Against this dire backdrop, we should be particularly attentive to the nutritional needs of women of color, particularly African Americans.
The burden of food insecurity is often disproportionately carried by BIPOC women. Contemporary and historical racial bias in healthcare may prevent some expectant mothers from being honest regarding experiencing food insecurity.21 To build trust, especially in medically underserved areas, the community voice should be integrated into programs. We should run programs for high-risk BIPOC pregnant women and their families to improve maternal and infant health by leveraging food- and education-based interventions. And by improving nutritional services for low-income women of color, we can lift standards for all expectant mothers in the U.S.
Collaboration and Community are Keys
There are several existing resources for expectant and new mothers provided at the federal, state, and local levels. At the federal level, there are cornerstone programs (e.g., Supplemental Nutrition Assistance Program; Special Supplemental Nutrition Program for Women, Infants, and Children) and key legislation (e.g., Mothers and Offspring Mortality and Morbidity Awareness Act; Oral Health for Moms Act) providing low-income pregnant women, new mothers, newborns, and young children with assistance. However, these resources have unfortunately not proven to be sufficient. We need additional, new initiatives and programs.
For any program design, we should incorporate the voices of patients and communities into the design. We should tailor initiatives to the needs of the specific communities being served, aiming to understand the characteristics of both the population currently being served and those who are not accessing the services. Effectively addressing the Social Determinants of Health (SDOH), including food security, requires collaboration and partnership with a variety of governmental, nongovernmental, and private sector entities. That is the key to incorporating diversity perspectives, overcoming capacity limitations, and expanding program scalability. To avoid duplication of effort or working at cross-purposes, we should conduct a thorough landscape scan of individuals and organizations already working to address this issue in a given community; we want to create a seamless network. These resources can provide deeper understanding and greater context of the actually lived experiences of those in the communities and neighborhoods.
We should particularly aim to partner with community leaders and local organizations. We should get communities involved in healthy food production and distribution. Local leaders can provide insights on culturally appropriate foods, norms, and traditions. Often times, some of the staff of local clinics, hospitals, and other medical facilities are (or were) members of the broader community the institution serves. These individuals are a great place to start the information gathering and knowledge expansion processes. In fact, some staff members will even occasionally meet eligibility criteria for enrollment in the program.
Best Practices for Programs
As we develop new initiatives, there are several best practices we should employ. Food should be healthy, accessible, easy to cook, and low-cost. We want to empower mothers with culturally competent nutrition information. Expectant women would benefit from food boxes, tailored meals, and specialty groceries. Additionally, they need access to cooking classes, cooking supplies, recipes, and ongoing nutrition counseling. It is important to translate nutritional guidelines into everyday practice; we can leverage community health workers and social workers for this purpose. Moreover, we should aim to treat whole families. For instance, family and other members of the household can also have a positive impact on the nutrition for both mother and child.
A sound meal delivery program should include a nutritious balance of dairy, fruits, proteins, and vegetables. The ideal nutrition plan includes fish, fruits, healthy fats with omega-3 fatty acids (e.g., nuts and seeds), legumes, oils rich in monounsaturated fat, and whole grains. The key is to consume more nutrient-dense, whole foods. Prudent nutrition featuring micronutrients and balanced protein energy has proven to improve birth outcomes, including reducing rates of low birth weight.22 Nutritional interventions should start as early in the pregnancy as possible and even during the preconception period. This helps mitigate more serious downstream complications for both mothers and children. And how can we reach mothers? We can leverage assets such as childcare, diaper banks, and free check-ups to gain access.
Beyond food, other social needs can be met using case management and social work approaches to address the Social Determinants of Health. The U.S. Centers for Disease Control and Prevention defines SDOH as the conditions in places where people live, learn, work, and play that impact a wide range of health risks, access, and outcomes.23 For example, we cannot overlook the role of exercise and physical activity during pregnancy and in the postpartum period; this activity can reduce adverse health outcomes. However, in order to exercise, the mother needs access to affordable, convenient, and safe facilities. This illustrates the interrelatedness of causal factors driving maternal health and well-being.
Effective and efficient screening is another recommended best practice. While many healthcare settings screen mothers for food insecurity, it is still not the norm. Women’s health providers, particularly those serving vulnerable populations, should consider adopting universal screening for maternal food insecurity. Frequently, those expectant moms most in need of a nutrition program are the same ones who struggle to find, join, and maintain participation because they suffer from the same barriers that generated the need in the first instance, so extra efforts must be made, including providing incentives (e.g., free diapers or baby clothes). Even if the screening is properly done and a need is identified, clinicians must connect patients to sources of healthy food. Thus, a strong network of private, public, and NGO sector suppliers/vendors is crucial.
Another key best practice is to incorporate the provider perspective. Why? Whether via in-person or virtual visits, healthcare providers are in an excellent (and unique) position to communicate with expectant mothers needing social supports, including food assistance, so we need to work at the point of care. Yet, medical providers often have hectic schedules, already laboring under an intense workload. Providers have to balance many competing demands, so any new initiative has to be cautious about creating additional staff burden. Beyond just implementing a raft of guidelines and mandates, we must make sure providers have adequate incentives and resources such as knowledge and time to discussion optimal nutrition with expectant mothers.
Conclusion
Improving maternal nutrition, including eradicating any food insecurity for pregnant women, is an amazing 2 for 1 public health opportunity. By addressing the new mother’s nutrition and wellness, we automatically improve that of the infant. And moreover, there are likely to be positive spillover effects to other members of the household who benefit from eating healthier. Conversely, failure to do this for the expectant/new mother has the real potential to consign her and the child to a lifetime of avoidable acute and chronic diseases.
Although the case for high quality nutrition for moms and babies is compelling from the humanitarian, public policy, and cultural/social perspectives, we know that is not always sufficient to garner funding and reimbursement. No matter how emotionally or intellectually compelling the pitch is for food-as-medicine for mothers/infants, it will not be financially sustainable unless it is economically compelling. We have to demonstrate that maternal nutrition can deliver a strong ROI for governments (e.g., Centers for Medicare & Medicaid Services), private insurers, and other payers. Thus, via actual application, demonstration projects, experiments, or pilots, we have to document evidence that this approach works, where “works” is defined as delivering short- and long-term savings that far exceed the short- and long-term costs.
We also should support the advancement of research focused on improving maternal health outcomes because there remain significant gaps in scholarly knowledge regarding nutrition during reproductive periods. For example, more research is needed on the consequences that food insecurity during pregnancy has on maternal and neonatal outcomes, and we should more scientifically determine indicators and predictors of preterm births. Academics have assembled many peer-reviewed studies establishing that medically tailored meals and food packages are effective in improving health outcomes,24 but this work is not specific to pregnancy-related outcomes for new mothers and infants. We will also need more research and tools for determining the ROI for maternity-related SDOH initiatives. Thus, fully implementing food-as-medicine for moms will take considerably more hard work, but the positive potential outcomes for mothers and for the most vulnerable in our society at the very start of their lives makes this a worthy fight.
About the Authors

James J. Gillespie, Ph.D., J.D., M.P.A., M.S.
Chief Health Officer, Umoja Food For Health
Senior Advisor and Strategy Consultant, Stanford University School of Medicine
Research Affiliate, Yale University School of Medicine
Co-Founder and Board Member, Black Healthcare and Medical Association
Advisory Board Member, Healthcare Businesswomen’s Association
Northwestern University Kellogg School of Management, M.S., Ph.D.
Harvard University School of Law, J.D.
Princeton University School of Public Policy, M.P.A.
Massachusetts Institute of Technology, B.S.
Carnegie Mellon University Heinz School; Rand Graduate School

Gregory J. Privitera, Ph.D., M.A.
Senior Advisor, Umoja Food For Health
Early Career Professional Presentation Award, American Psychological Association
Most Promising New Textbook Award, National Winner, Text and Academic Authors Association
Best-selling book on SAGE list for general statistics market
Published more than a dozen books in statistics, methodology, strategic analytics, behavioral health, and healthcare
More than 200 institutions have adopted his books, including Columbia, Darthmouth, Harvard, Johns Hopkins, and Stanford
Quoted in The Wall Street Journal, The Huffington Post, Time Magazine, and Oprah’s Magazine
Board of Directors, Olean General Hospital Foundation, and the Center for Women in Healthcare and Life Sciences
Arizona State University, Postdoctoral Associate
University of New York at Buffalo, Ph.D. in Behavioral Neuroscience and Psychology, M.A., B.A.

